Evaluating Patient Reported Obstetrical History at Initial Prenatal Visit
Micah R. Wright DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United States
Thanh Luu DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United States
Katie Smith, Oklahoma State University Center for Health Sciences Tulsa, OK United States
Jessie Sorelle, Oklahoma State University Center for Health Sciences Tulsa, OK United States
Christa Sikes DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United States
Anne Bowes DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United
States
DJ Vargas DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United
States
Carlos Guevara DO, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK
United States
Lance Frye MD, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK United
States
William Po MD, Oklahoma State University Medical Center Department of OB/GYN Tulsa, OK, United
States
Abstract
Aim
The potential for recall bias at initial intake visit of multiparous obstetrical patients is a common concern. Accuracy of initial obstetrical history reporting can drastically alter the course of pregnancy management if the information documented during the current gestation is inaccurate. This retrospective study assesses the overall accuracy of obstetrical history reporting at intake visit for multiparous obstetrical patients.
METHODS
Delivery record data from our urban-centered academic teaching institution was collected from January 2016-February 2018. Research collection included specific patient-reported obstetrical history. Delivery records were screened by all authors and EMR delivery record data was compared with the initial obstetrical history comparison of accuracy.
RESULTS
321 delivery records were retained for final analysis. Of these, 318 (99%) recorded accurate type of delivery, 301 (94%) accurately recorded year of delivery, 292 (91%) accurately recorded gravida and para history, 208 (65%) reported accurate gestational age at delivery, and 186 (58%) accurately recorded birth weight. Fifty antepartum complications were documented in the EMR. Of the fifty documented antepartum complications, thirty-five (70%) of those complications were reported. Thirty-one delivery complications were documented in the EMR. Of those thirty-one, patients reported twelve (39%) complications. Within this subset, nineteen vaginal and/or perineal lacerations were documented with only two (1%) reported. Fifteen postpartum hemorrhages were documented with six (40%) reported, and seven incidents of shoulder dystocia were documented with four (57%) reported.
CONCLUSION
Results suggest our patient population was accurate at recording routine obstetrical information on initial prenatal visit. However, poor accuracy was noted in reporting of detailed obstetrical information with potential for significant impacts on management of future pregnancies. Results obtained from this study can create measures to improve patient's obstetrical history reporting.
Keywords: Obstetrics, Clinical Obstetrics, Obstetrical History, Labor and Delivery, Delivery Records, Obstetrical complications, Antenatal care
Introduction
Obstetrical management of a patient can be highly dependent on prenatal and perinatal factors in previous pregnancies, such as neonatal age, gestational weight, mode of delivery, complications during delivery, and postpartum complications. Recall bias is a common concern throughout obstetrics and many studies have been done to evaluate accuracy of patient recall in all areas of medicine. The history documented during an initial obstetric visit is often conveyed by the patient and typically assumed to be accurate1. Previous studies investigating this topic used wide-ranging classifications for mode of delivery such as caesarean section versus 'not caesarean section1.
However, research specifically on the ability of women to recall the events of their pregnancy, labor and birth, and child's early infancy have yielded mixed results2.
The magnitude of potential complications resulting from inaccurate history reporting has led our team to question what variables in history taking yield such results. Previous studies have found that the degree of accuracy fluctuates with the amount of medical vocabulary utilized, the style of questioning, the time frame between event and survey, and perceived importance of event to participants2 &17. Inaccurate history can lead to mismanagement of the patient as well as the potential for physician error18. Access to obstetrical records and evaluation of the quality of patient self-reported obstetrical history continues to remain a growing concern among providers involved in obstetrical care. Improper management of high-risk obstetrical patients secondary to inaccurate obstetrical history can lead to potential fatal complications in the later stages of obstetrical care if certain preventative screens, measurements, and guidelines are not implemented early on in patients antepartum care. As such, retrospective reviews remain a feasible option for information analysis 19. Retrospective reviews of patient medical records could provide avenues for physicians to obtain information on missed medical diagnoses and complications noted during previous pregnancies. Obtaining such information early in antepartum care allows the obstetrical care team to be proactive in treating and preventing severe morbidity and mortality in high risk patients. The purpose of this study is to utilize electronic medical records to compare a patient's obstetric history provided at the intake visit with the documented electronic delivery data in order to ascertain the validity of the individual's recall with an aim to prove that thorough obstetrical history review can provide an insight into managing potentially missed high risked obstetrical patients.
Methods
Oversight and Reporting
This study was subject to an expedited Institutional Review Board oversight and did not meet the regulatory definition of human subject research as defined in 45 CFR 46.102(d) and (f) of the Department of Health and Human Services' Code of Federal Regulations [7]. We reviewed several sources when developing the methodology for this study.
Delivery record data from one urban-centered academic teaching institution was collected from January 2016-Febuary 2018 (time frame of our current EMR use within the department clinic). This list was generated from the HIT department at our delivering institutions. The same patients who had obtained prenatal care at the outpatient facility for their subsequent pregnancies were included in the study. Initial intake visit information was collected by a questionnaire and completed during patient's initial intake visit. From this same list, patient medical record numbers were used to identify charts then discarded from data collection. De-identified information provided from patient charts for research collection included the following patient-reported obstetrical history:
• Gravidity and parity history
• Type of delivery- cesarean section, spontaneous vaginal delivery or operative vaginal delivery
• If cesarean section or operative vaginal delivery, what was the indication
• Delivery date
• Gestational age at delivery
• Birth weight
• Antepartum complications (hypertension, history of preeclampsia in previous pregnancy, diabetes mellitus type 1 or 2, and gestational diabetes)
•Delivery complications (perineal/vaginal lacerations, post-partum hemorrhage, incidents of shoulder dystocia)
All recorded information was stored in a locked area within the clinic accessible to clinical investigators (Micah Wright, Thanh Luu, Anne Bowes, Christa Sikes, Jessie Sorelle and Katie Smith). Once data collection was finished, patient information was de-identified.
Screening Records for Eligibility
Six investigators (MW, TL, AB, CS, JS and KS) screened delivery records retrieved from the initial electronic medical record searches for relevance. First, these investigators evaluated whether the delivery records indicated that patients had received prenatal care at our clinic. Records without mention of prenatal care were initially separated for further investigation, and patients with documented prenatal care at our clinic were retained. Records with unclear relevance were reviewed by MW, KS and JS. To qualify for inclusion, the delivering patient must have filled out an initial intake obstetrical history report or have transfer of care delivery records. Patients were excluded if either the delivery record or the initial intake history was not available. For this study, we did not include early first trimester losses (gestational age under nine weeks) as we did not have the ability to cross-reference the accuracy of reported history with the electronic medical record (EMR) systems. The final list of medical records included in analysis was verified independently by two co-authors with identical inclusions. Next, charts of currently pregnant individuals receiving prenatal care were reviewed for previous deliveries at our hospital. If these criteria were met, then intake history in our clinic was compared with the patients delivery record for comparison of accuracy in data reporting. Near-accurate information in reporting was recorded as inaccurate in final analysis.
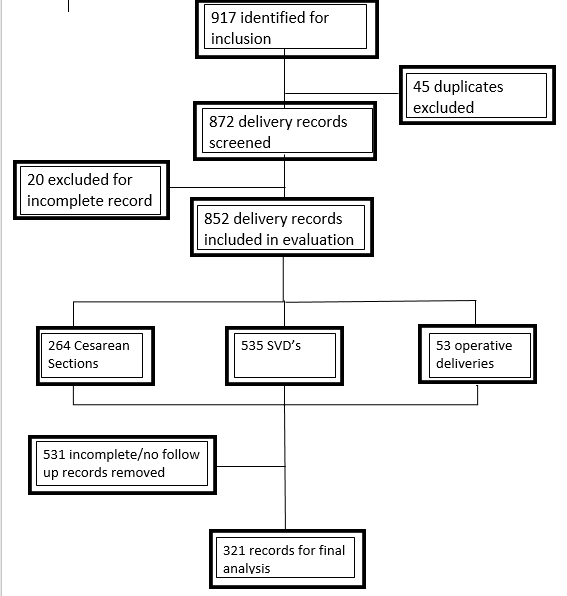
Between January 2016 and February 2018 there were 917 deliveries recorded in our delivering institution's EMR. Of these 917 delivery records, we initially excluded 45 due to duplication of delivery record. 872 delivery records were retained for initial screening and included in evaluation. After initial screening to determine if delivery records qualified for inclusion, 20 studies were excluded for incomplete delivery information. A total of 852 delivery records identified, 264 cesarean sections, 535 spontaneous vaginal deliveries, and 53 operative vaginal deliveries were performed. After thorough evaluation, 531 delivery records were excluded secondary to incomplete initial intake obstetrical history or no obstetrical follow-up in the postpartum periods for the subsequent pregnancy. The characteristics in the excluded studies did not differ from those that were included within the study.
Results
A total of 321 delivery records were retained for final analysis (Figure 1).
Figure 1.
Of these remaining records, 318 (99%) accurately recorded the type of delivery (when compared to electronic medical record), 301 (94%) accurately recorded year of delivery, 292 (91%) accurately recorded gravida and para history, 208 (65%) reported accurate gestational age at delivery, and 186 (58%) accurately recorded neonatal weight at delivery. All of these percentages were compared to the data that was provided by the EMR system.
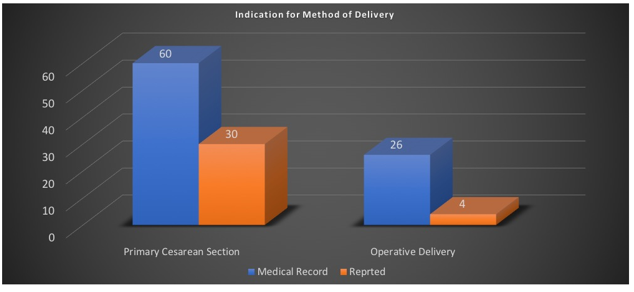
Of the 318 patients who accurately reported the type of delivery, sixty patients were recorded to have primary cesarean sections. Of those sixty, thirty (50%) patients reported accurate indication for primary cesarean section. Twenty-six patients were recorded to have operative vaginal deliveries. Of those twenty-six, four (15%) patients reported accurate indication for operative vaginal delivery. (Figure 2)
Figure 2.
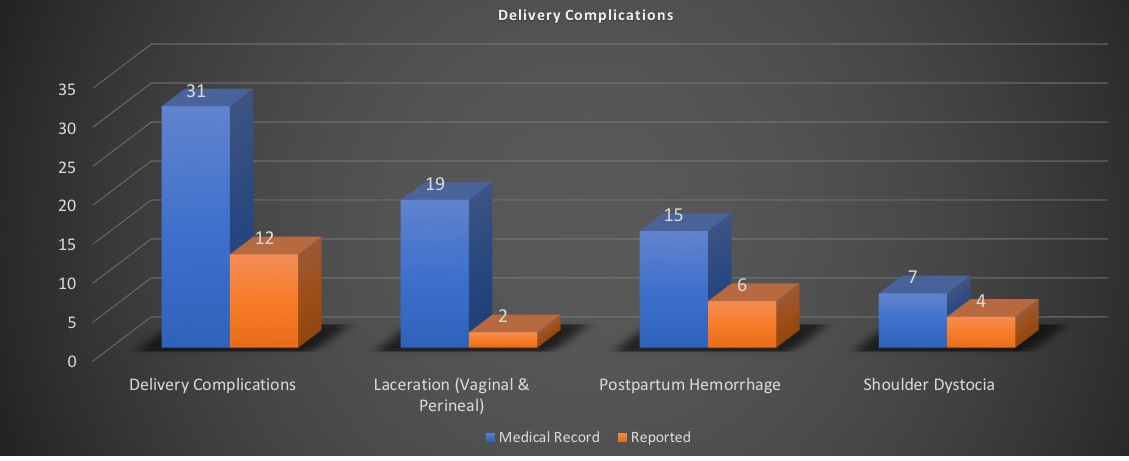
Thirty-one delivery complications were documented in the EMR. Of those thirty-one, patients reported twelve (39%) complications. Within this subset, nineteen vaginal and/or perineal lacerations were documented with only two (1%) reported. Fifteen postpartum hemorrhages were documented with six (40%) reported, and seven incidents of shoulder dystocia were documented with four (57%) reported. (Figure 3)
Figure 3
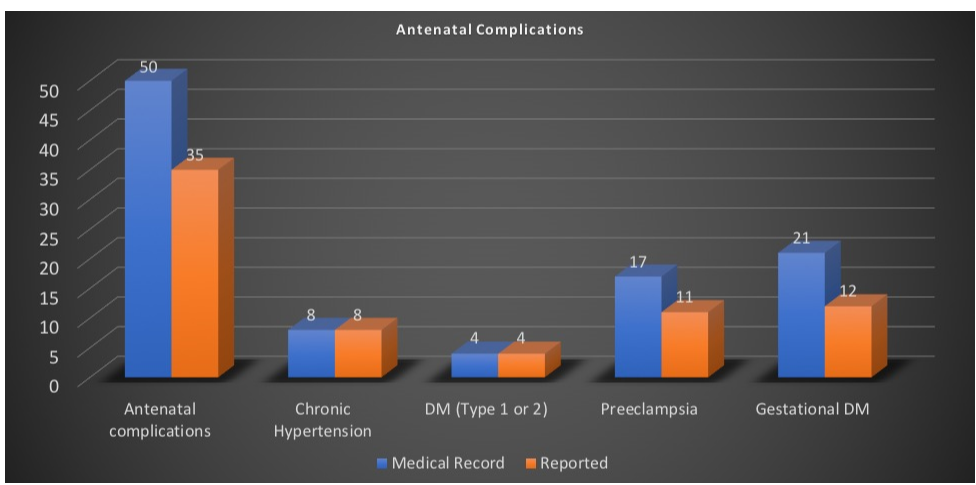
Of the 321 delivery records, fifty antepartum complications were documented in the EMR. Of the fifty documented antepartum complications, thirty-five (70%) of those complications were reported. Of this subset, eight records indicated chronic hypertension with all reporting this diagnosis, four records indicated diabetes mellitus, type 1 or 2, with all reporting diagnosis, seventeen records indicated a history of preeclampsia with eleven (65%) accurately reporting this diagnosis, and twenty-one records indicated history of gestational diabetes with only twelve (35%) reporting the diagnosis. (Figure 4)
Figure 4.
Of the 321 delivery records, 22 preterm deliveries were documented, with fourteen (63%) reporting history of preterm delivery, and only five (23%) records reporting known cause of preterm delivery. Of the remaining 299 delivery records documenting term delivery, fifteen (5%) inaccurately reported preterm delivery.
Discussion
In our current medical society, many studies have used interviews to obtain a patient's medical history. Conversely, the validity of these self-reporting surveys is often not evaluated in terms of their accuracy3. Our study assessed the accuracy during reporting of obstetrical history for obstetrical patients returning for subsequent prenatal care. The results from the study yielded a few different outcomes from the 321 delivery records that were reviewed. Overall, women were generally accurate in reporting chronic or personal aspects of their medical history. This is consistent with a previously published study by Kehoe et al, 1994 where subjects were able to accurately recall their medical and drug history in well-defined chronic conditions. These conditions in our current study included the type of delivery, the year of delivery, gravidity and parity, chronic hypertension, and diabetes mellitus. In our study, these five facets were accurately reported in greater than 90% of our study pool. This supports previously published literature that maternal reporting of the aforementioned aspects can be used with credence.
However, in contrast to the previously mentioned characteristics, our study showed features that are relatively more acute (those occurring during labor and delivery) were less accurately recalled. These included gestational age at delivery, birth weight, indication for primary cesarean section, indication for operative vaginal delivery, antepartum complications (preeclampsia and GDM), intra and post-partum complications (lacerations, post-partum hemorrhage, and shoulder dystocia), and preterm delivery. The validity of these complications ranged from 1% to 65%. With these factors, it may be useful for the clinician to probe the patient at her initial visit to ascertain a clearer picture of her obstetrical history and further guide decisions using evidence-based medicine for current and future pregnancies.
Current research studies may underestimate the accuracy of maternal self-reporting. This may be attributed to innate flaws in data collection and assumptions. One of these flaws includes the assumption that medical records are a perfect source of data. Secondary to incidental input errors (EMR templates, free-hand input), transfer of information (dictations), and human errors, medical records may not be the gold standard of accurate patient data. Additionally, aspects that our study did not evaluate were demographic factor associated with maternal education level achieved and depth of counseling provided by their physician during both antenatal care and delivery. This may be a contributing factor in more accurate recall of more transient events (i.e., pregnancy-related diseases).
Our study has several strengths, but most notably is the ability to be easily replicated. We used duplicate data extraction, with all data being extracted and verified by multiple members of the research team. Our study also has several limitations in both design and execution. With access only to a limited sample size of one delivering institution, our patient population may not provide an accurate general representation of a typical obstetrical population. Several medical records we encountered were partially incomplete. Finally, our study may have indicated that hospital records are the gold standard and without fault, which is not the intended purpose.
Our study should encourage conversation about the best practices to improve patient knowledge of critical factors that could affect the course of their prenatal care. Results from this study will be used to improve obstetrical history reporting and will aid in creating measures to extract delivery data prior to seeing patients at initial prenatal visits. This data will be used in a prospective case study in which real-time education will be carried out in the immediate postpartum and 6-week post-partum visits. This real-time education will detail specific events that occurred during labor and delivery as well as in the intrapartum and post-partum period. Further studies will be performed in order to assess if patient reporting of obstetrical history can be improved with overview of previous pregnancy obstetrical history.
Author Contributions:
All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; gave final approval of the version of the article to be published; agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgements:
The authors would like to thank the Oklahoma State University Center for Health Sciences Department of Obstetrics and gynecology.
Disclosure statement:
The authors declare that they have no conflicts of interest and nothing to disclose.
References
1. MA Quigley, C Hockley, LL Davidson. Agreement between hospital records and
maternal recall of mode of delivery: Evidence from 12 391 deliveries in the UK Millennium Cohort Study. BJOG an International Journal of Obstetrics and Gynaecology. 2006. 114(2):195-200.
2. Githens PB, Glass CA, Sloan FA, Entman SS, Maternal Recall and Medical Records: An Examination of Events During Pregnancy, Childbirth, and Early Infancy. Birth 1993; 20(3): 136-141.
3. Harlow SD, Linet MS. Agreement between questionnaire data and medical records: The evidence for accuracy of recall. A m J Epidemiol 1989;129(2):233-248.
4. Krall EA, Valadian I, Dwyer JT, Gardner J. Accuracy of recalled smoking data. Am J Public Health 1989;79(2):200- 206.
5. Mackenzie SG, Lippman A. An investigation of report bias in a case-control study of pregnancy outcome. Am J Epidemiol 1989;129(l):65-75.
6. Chu SY, Lee NC, Wingo PA, Webster LA. Alcohol consumption and the risk of breast cancer. Am J Epidemiol 1989;130(5):867-877.
7. Giovannucci E, Colditz G, Stampfer MJ, et al. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol 1991;133(8):810-817.
8. Loftus ER, Fathi DC. Retrieving multiple autobiographical memories. Social Cognition 1985;3(3):280-295.
9. Mitchell AA, Cottler LB, Shapiro S. Effect of questionnaire design on recall of drug exposure in pregnancy. Am J Epidemiol 1986;123(4):670-676.
10. Sokol RJ,Martier SS, Ager JW. The T-ACE questions:Practical prenatal detection or risk-drinking. Am J Obstet Gynecol 1989;160(4):863-870.
11. Bean JA, Leeper JD, Wallace RB, Sherman BM, Jagger H. Variations in the reporting of menstrual histories. Am J Epidemiol 1979;109(2): I81- 185.
12. Martin CJ. Monitoring maternity services by postal questionnaire: Congruity between mothers' reports and their obstetric records. Stat Med 1987;6(5):613-627.
13. Means B, Nigam A, Zarrow M, Loftus EF, Donaldson MS. Autobiographical memory for health-related events. In: Keppel KG, Heuser RL, Placek PJ, et al, eds. Methods and Response Characteristics. 1980 National Natality and Fetal Mortality Surveys. Vital and Health Statistics, series 2, no. 100, DHHS pub. no. (PHS) 86-1374. Washington, DC: National Center for Health Statistics, Government Printing Office 1986; l-27.
14. Oates RK, Forrest D. Reliability of mothers' reports of birth data. Aust Paediatr J 1984;20(2):185-186.
15. Wilcox AJ, Horney LF. Accuracy of spontaneous abortion recall. A m 7. Epidemiol 1984;120(5):727-733.
16. Robert Kehoe, Suh-Yuh Wu, M. Cristina Leske, and Leo T. Chylack, Jr. Comparing Self-reported and Physician-reported Medical History American Journal of Epidemiology, Vol 139, 813-818
17. Stephen L. Bukaa, *, Jill M. Goldsteinb,c, Eleni Spartosa, Ming T. Tsuangb,d The retrospective measurement of prenatal and perinatal events: accuracy of maternal recall Schizophrenia Research 71 (2004) 417-426
18. Keenan K, Hipwell A, McAloon R, et al. Concordance between maternal recall of birth complications and data from obstetrical records. Early Hum Dev 2017 Feb; 105:11-15. doi: 10.1016/j.earlhumdev.2017.01.003