Examination of maternal mortality risk factors among pregnant women in the United States: A cross-sectional analysis of BRFSS 2017-2019
Mariama Abramson, B.S., Oklahoma State University College of Osteopathic Medicine, Tulsa, Oklahoma
Vanessa Lin, BA., Oklahoma State University College of Osteopathic Medicine, Tulsa, Oklahoma
Jordyn Austin., B.S., Oklahoma State University College of Osteopathic Medicine at Cherokee Nation, Tahlequah, Oklahoma
Marshan Marick, DrPH., Oklahoma State University, Department of Health Education and Promotion, College of Education and Health Sciences. Tulsa, OK
Micah Wright, D.O., Oklahoma State University Center for Health Sciences, Department of Obstetrics & Gynecology, College of Osteopathic Medicine. Tulsa, OK
Benjamin Greiner, D.O, MPH., University of Texas Medical Branch, Department of Internal Medicine, Galveston, Texas
Micah Hartwell, Ph.D., Oklahoma State University College of Osteopathic Medicine & Oklahoma/ Oklahoma State University Center for Health Sciences, Department of Psychiatry and Behavioral Sciences, Tulsa, Oklahoma
Abstract:
Background:Chronic conditions including hypertension, hypercholesterolemia, and diabetes mellitus can lead to maternal death. The last study to investigate the prevalence of these risk factors among pregnant women was published in 2011; thus, the objective of this study was to update the literature regarding these risk factors and associated behaviors.
Methods: Combining 2017, 2018, and 2019 Behavioral Risk Factor Surveillance System datasets, we estimated the prevalence of chronic comorbidities, and calculated adjusted odds ratios (AOR) between disease and health-related risk factors.
Results: High cholesterol was the most prevalent risk factor—11.2% followed by diabetes at 9.6%. The health-related risk factor most related to comorbidities was physical inactivity (28.9%). Age was significantly associated with all three chronic conditions
Conclusions: Risk factors for childbirth and maternal mortality were more prevalent among women bearing children later in life, and Black and Hispanic pregnant women were more likely to have risk factors associated with these conditions.
Introduction
Each year in the United States (US) hundreds of women die from pregnancy-related deaths that are largely preventable. Contrary to the trends present in countries outside the US, these numbers are on the rise. Between 1990 and 2013, there was a 44% decrease in global maternal mortality; however, the US saw a 1.7% increase in mortality rising from 10 deaths per 100,000 live births to 17.3.1 This discrepancy between U.S. and global maternal mortality rates is partially due to changes in US policy and differences in worldwide reporting standards.2 Although the US definition of maternal mortality is more inclusive than that of the World Health Organization - death within 1 year of pregnancy compared to within 42 days of pregnancy - the difference in mortality can be partially explained by worsening overall health within the US, widening gaps of health disparities, and increasing maternal age.3,4
Chronic disease rates among women of reproductive age have increased in the United States, with approximately 27% of pregnancies affected by a chronic disease. 5Although there are a wide range of factors that can predispose women to maternal mortality, cardiovascular issues tend to be the cause for a large number of reported maternal deaths. In 2018, state-based maternal mortality review committees (MMRCs) from nine states reported that cardiovascular conditions were included in the main causes of 50% of pregnancy-related deaths and CDC data from 2019 supported this as well, showing about 33% of these deaths being due to cardiovascular conditions.6
First, as hypertension is the leading risk factor for heart disease and stroke,7 it is also a major contributing factor to maternal and fetal morbidity, complicating up to 5% of the estimated 4 million pregnancies in the United States annually.8 Next, obesity is considered an identifiable risk factor for cardiovascular disease, predisposing women to pregnancy-related death. In addition to predisposing women to cardiovascular disorders, obesity also puts them at risk for other pregnancy complications such as preeclampsia, gestational diabetes, and metabolic disorders.9 Nearly half of women of child-bearing age are either overweight or obese10— conditions which have long been known to complicate pregnancy and delivery, and are associated with increased morbidity for both the mother and the child,11
Increasing trends in the rates of obesity, hypertension, and coronary artery disease are accompanied and amplified by increasing maternal age.1 Maternal age has been shifting upward over the past 50 years, with a 2015 study reporting nearly 3% of expecting women being over the age of 40.1 In combination with the increased prevalence of comorbidities past the age of 30, an estimated 50% of all pregnancy-related mortality occurs after this age.12 Compared to a 20-year-old woman, the odds are 5 times more likely that a woman in her 30’s will die during pregnancy or within a year of giving birth.13 Risk factors for maternal mortality include physical health, age, and healthcare disparities in minority and low socioeconomic status groups.14
Compared to White women, Black women are two to three times more likely to die from pregnancy-related complications— which doubles in risk as they pass the age of 30.15 Further,
the risk of death from pregnancy-related complications for women who identify as American Indian or Native Alaskan was nearly as high as their Black counterparts.
15 The increased likelihood of pregnancy-related death among minorities is linked to increased prevalence of chronic disease,16 advanced states of these diseases,17 lack of access to health care, and the quality of care.18
In addition to maternal mortality, these same conditions account for an additional 60,000 women requiring emergency surgeries during birth or being diagnosed with a life-threatening condition during their pregnancy.19 As the rates of mortality and hospitalization are commonly assessed in the US, to our knowledge there have been no recent studies that have assessed the prevalence of maternal mortality risk factors among pregnant women in the US. Therefore, the objective of this study was to use a nationally representative sample of the US population to assess the prevalence of comorbidities related to maternal mortality and assess the socioeconomic and lifestyle factors that predicate these risks.
Methods
A cross-sectional study design was used to analyze a combined dataset consisting of 2017, 2018, and 2019 Behavioral Risk Factor Surveillance System (BRFSS) surveys. BRFSS is a Centers for Disease Control and Prevention operated database publishing self-reported, health behavior, and diagnosis related surveys. Using a complex randomized sampling technique which had been previously validated by BRFSS, surveys were collected from all 50 states plus the District of Columbia, Puerto Rico, and Guam. Informed consent was obtained prior to survey completion. This manuscript was developed in adherence to the recommendations published by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.20 Our study utilized publicly available, de-identified data and therefore the an institutional review board determined this study did not constitute human subjects research.
Participants were included if they answered “Yes” to the question: “To your knowledge, are you now pregnant,” which was asked of all women between 18 and 49 years of age. Respondents that were institutionalized, living in military barracks, males, and non-pregnant females were excluded. Extracted data consisted of socio-demographic variables including race, age, income, marital status, number of children in the household, current healthcare coverage, lifestyle behaviors including physical inactivity (sedentary), current smoking status, and alcohol consumption, and the presence of chronic conditions including hypertension, hypercholesterolemia and diabetes mellitus (including prediabetes and gestational diabetes).
Smoking status is a calculated, binary variable in BRFSS distinguishing between individuals who currently smoke and those who are former smokers or non-smokers. Sedentary behavior was coded as a binary variable based on the question, “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?” Alcohol consumption is a calculated, binary variable in BRFSS reporting affirmative if an adult reported having at least one drink of alcohol within the past 30 days. Healthcare coverage was coded as a binary variable with those answering “Yes” of “No” to the following question: “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare, or Indian Health Service?” Marital status was extracted from the BRFSS survey item which collected individuals relationship status which included options of “Married,” “Divorced,”“Widowed,” “Seperated,” “Never married,” and “Member of a non-married couple.” A status of ‘married’ has been shown to be significantly associated with better outcomes compared to other statuses,
21 thus for statistical parsimony, we coded this as a binary variable. Chronic diseases were coded as binary variables if the individual reporting having been diagnosed with the condition.
We first calculated population estimates of demographic characteristics and prevalence rates of the health-related risk factors. Next, multivariable logistic regression models were constructed to determine associations, via adjusted odds ratios (AOR), between chronic disease (hypertension, hypercholesterolemia, and diabetes) and demographic and health-related risk variables. Next, to assess differences in health-related risk factors by race, we constructed a multinomial logistic regression model and examined associations disparities in healthcare coverage, marital status, education, sedentary behavior, alcohol consumption, and smoking via relative risk ratios (RRR). Sampling weights, provided by BRFSS, were adjusted for the combined datasets. Alpha was set at .05, hypotheses were two-sided, and statistical analyses were performed using Stata 16.1 in December 2020.
Results
Demographics of respondents
Response rates for BRFSS were approximately 50%, with a total number of respondents in the combined datasets being 1,305,720. After excluding men and non-pregnant women, 7,101 women were included in this sample, representing a population estimate of 2,308,485. Of these women, 53.3% were between the age of 18 and 29, 27.7% were between 30 and 34 years of age, and 19.0% were over the age of 35 (Table 1). The race and ethnicity of the sample consisted of 49.2% White women, 13.0% Black women, 7.3% Asian women, and 1.5% American Indian or Native Alaskan women. While 32.8% reported having no children, 29.4% reported having 1 child, and 37.88% reported having 2 or more children. Nearly 59.5% of respondents reported attending some college, 57.5% were married and 13% lacked healthcare coverage.
Prevalence of health-related risk factors for maternal mortality
The most prevalent behavioral risk for comorbidities among pregnant women was physical inactivity (28.9%). Additionally, 13.0% of women said they had consumed alcohol in the past 30 days, and 7% said they had smoked tobacco during this time frame (Table 1).
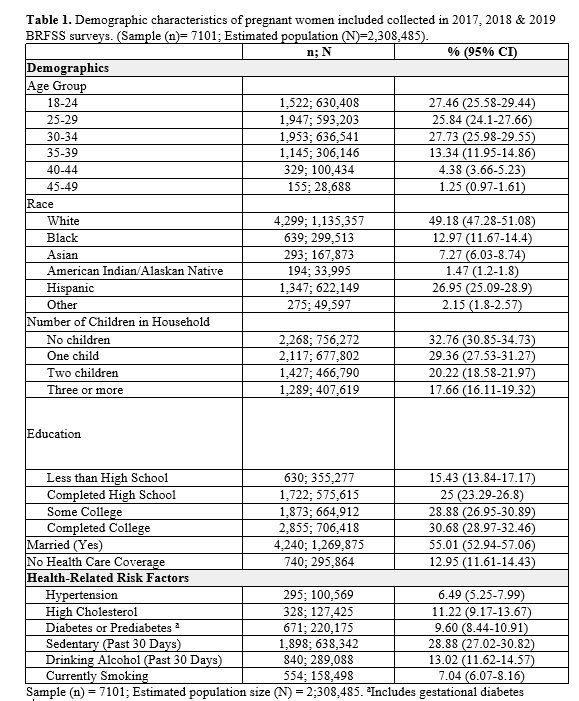
The most prevalent chronic condition was hypercholesterolemia (11.2%) followed by diabetes mellitus (9.6%) and hypertension (6.5%).
Associations of socio-demographics and chronic conditions among pregnant women
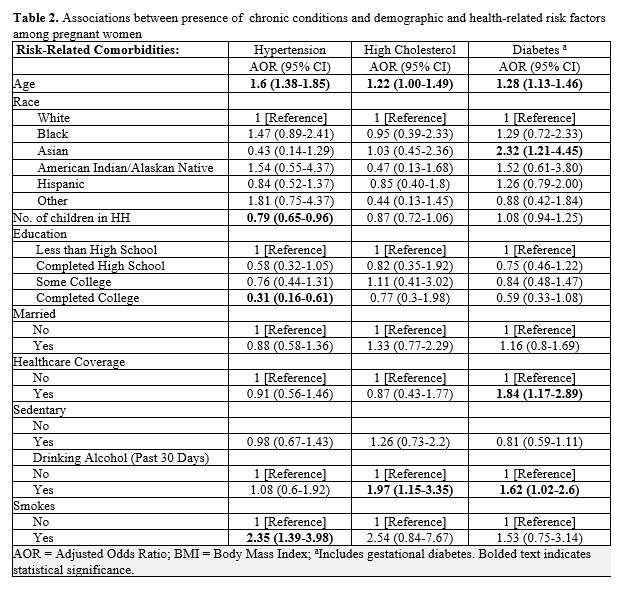
Age was a consistent risk factor for chronic conditions across hypertension (AOR: 1.60; 95%CI: 1.38-1.85), hypercholesterolemia (AOR: 1.22; 95%CI: 1.00-1.49), and diabetes (AOR: 1.28; 95%CI: 1.13-1.46) among pregnant women (Table 2). Other statistically significant associations were found between hypertension and the number of children currently in the household (AOR: 0.79 95%CI: 0.65-0.96) — showing lower odds of having hypertension with more children and having a college degree (AOR: 0.31; 95%CI: 0.16-0.61). Alternatively, being a current smoker increased the odds of having hypertension (AOR: 2.35; 95%CI: 1.39-3.98). Significant factors associated with a diabetes diagnosis among pregnant women were having healthcare coverage (AOR: 1.84; 95%CI: 1.17-2.89), drinking alcohol within the past 30 days (AOR: 1.62; 95%CI: 1.02-2.60), and being Asian American (compared to White women, (AOR: 2.32; 95%CI: 1.21-4.45).
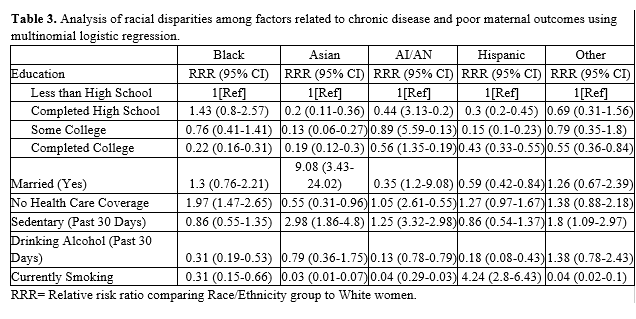
Using White women as the reference model, our final analysis showed that Black women were less likely to be married (RRR: 0.22; 95%CI: 0.16-0.31), more likely to have a high school diploma as their highest level of education (RRR: 1.87, 95%CI: 1.47-2.65), more likely to be sedentary (RRR: 1.97; 95%CI: 1.47-5.65), and less likely to smoke (RRR: 0.31; 95%CI: 0.19-0.53). Asian American women were more likely to have been sedentary (RRR: 1.65; 95%CI: 1.05-2.61) and have consumed alcohol (RRR: 2.03; 95%CI: 1.25-3.31) in the past 30 days, and were less likely to have smoked (RRR: 0.32, 95%CI: 0.13-0.78). Indigenous Americans were more likely to have healthcare coverage (RRR: 9.08; 95%CI: 3.43-24.02) and to have consumed alcohol (RRR: 2.98; 95%CI: 1.86-4.80) while being less sedentary (RRR: 0.55; 95%CI: 0.31-0.96) and less likely to have completed high school. Hispanic women were less likely to have healthcare coverage (RRR: 0.59; 95%CI 0.42-0.84), be married (RRR 0.43; 95%CI: 0.33-0.55), have completed high school, attended college, or have a college degree, and were less likely to smoke (RRR: 0.18; 95%CI: 0.08-0.43). Respondents identifying as ‘other’ were less likely to be married (RRR: 0.55; 95%CI: 0.36-0.84).
Discussion
Our study adds to the complexity of identifying characteristics and risk factors for maternal mortality. For instance, we found that having existing children in the household was correlated with a lower incidence of hypertension and that having healthcare or being Asian American increased the likelihood of having a diabetes diagnosis—while Asian American women are generally perceived to be healthier than other races, previous research has shown they may be prone to gestational diabetes due to differences in glucose metabolism and insulin response.22,23 Other studies in this area, focusing on individual conditions like diabetes or lifestyle behaviors 24–27, produced results in line with ours regarding smoking, alcohol, physical activity, and education; however, few have looked at lifestyle behaviors as a link between chronic disease among pregnant women— especially among a nationally representative dataset.
A common risk factor— age— was associated with being diagnosed with each of the chronic diseases we examined. For several decades, maternal age has been shifting upwards as more women choose to postpone their first pregnancy.28 Despite making up a smaller percentage of pregnancies, previous research has shown that pregnant women aged 35 or above account for approximately 30% of pregnancy-related deaths.12,13 With the continued advances in the field of reproductive medicine, it is very likely that maternal age will continue to increase. Pregnancies complicated by advanced maternal age require more frequent prenatal visits and neonatal screening to predict or help prevent maternal morbidity and mortality. With the knowledge that the majority of maternal deaths are linked to cardiovascular disorders related to preventable chronic conditions, it is important to observe this group closely and identify opportunities throughout the course of prenatal care to improve their maternal outcomes.
Further, our results also showed that more than one in 10 pregnant women lacked healthcare coverage and that race was linked to a number of underlying risk behaviors — in line with other research.7,8,11,23 The convergence of socioeconomic and lifestyle factors’ impact on maternal mortality is shown in our examination of racial disparities. Black women were less likely to be married and have attended higher education. A similar trend was also found among Hispanic women in addition to having a lower prevalence of healthcare coverage. These factors likely demonstrate greater financial stress during pregnancy. Additionally, Black and Asian American women were less likely to report exercising in the past 30 days— a known risk factor for cardiovascular disease.29,30,31, Indigenous women completed lower levels of education compared to White women but were more likely to have healthcare coverage, likely due to tribally affiliated healthcare.
To generate preventive interventions, it is necessary to develop a clear understanding of the underlying mechanisms that create these health disparities. The connection between income and access to care has been identified,32 yet remains an important consideration for improving maternal mortality rates. For instance, one important clinical aspect to decrease maternal morbidity is to address the lack of care in the immediate postpartum period through the appropriate transition of care after birth, especially in women with hypertension, metabolic syndrome, and other cardiovascular disorders.
To improve maternal mortality rates, it is imperative that efforts extend beyond clinical care delivery strategies to also embrace solutions that address the systemic issues which influence care delivery. By addressing systemic issues in education and healthcare, it may be possible to decrease the prevalence of chronic diseases19 that are risk factors for pregnancy complications. The nature of healthcare in the US makes it difficult to implement nationwide standardized maternity guidelines; thus, the best opportunity to affect change may be at the state or community level19 since states can contribute to improvements in maternal health. Policy recommendations at the state and local level can be customized to leverage data and resources to address systemic issues that impact maternal care delivery and outcomes.
This study had several strengths and limitations. Limitations of this study included a moderate response rate among BRFSS surveys. Additionally, the study questionnaire was self-reported, and therefore, response bias may have negatively affected our results. Furthermore, diabetes mellitus type 1 and 2 were not differentiated by BRFSS which may have skewed our results regarding this diagnosis. Finally, this was a cross-sectional analysis; thus, causation statements cannot be made. Study strengths included the large sample size and robust sampling procedures.
Conclusion
This study identified key characteristics and risk factors for maternal mortality in the US demonstrating that a closer examination of these disparities may be useful in making necessary changes in local, state, and national level public health initiatives. Increasing maternal age is a known risk factor for hypertension, hypercholesterolemia and diabetes among pregnant women; addressing lifestyle behaviors, socio-economic issues, and racial disparities linked to these chronic diseases may reduce the risk of severe complications and deaths during pregnancy and childbirth.
Acknowledgements: Not applicable
References
1. Kilpatrick SJ. Next steps to reduce maternal morbidity and mortality in the USA. Womens Health. 2015;11(2):193-199.
2. De Brouwere V, Tonglet R, Van Lerberghe W. Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the industrialized West? Trop Med Int Health. 1998;3(10):771-782.
3. Neggers YH. Trends in maternal mortality in the United States. Reproductive Toxicology. 2016;64:30-31. doi:10.1016/j.reprotox.2016.06.065
4. Ozimek JA, Kilpatrick SJ. Maternal Mortality in the Twenty-First Century. Obstet Gynecol Clin North Am. 2018;45(2):175-186.
5. Tyer-Viola LA, Lopez RP. Pregnancy with Chronic Illness. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2014;43(1):25-37. doi:10.1111/1552-6909.12275
6. Collier A-RY, Molina RL. Maternal Mortality in the United States: Updates on Trends, Causes, and Solutions. Neoreviews. 2019;20(10):e561-e574.
7. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Division of Behavioral and Social Sciences and Education; Board on Children, Youth, and Families; Committee on Assessing Health Outcomes by Birth Settings, Backes EP, Scrimshaw SC. Maternal and Newborn Care in the United States. National Academies Press (US); 2020.
8. Varagic J, Desvigne-Nickens P, Gamble-George J, et al. Maternal Morbidity and Mortality: Are We Getting to the “Heart” of the Matter? J Womens Health . 2021;30(2):178-186.
9. Pantham P, Aye ILMH, Powell TL. Inflammation in maternal obesity and gestational diabetes mellitus. Placenta. 2015;36(7):709-715.
10. Vahratian A, Zhang J, Troendle JF, Savitz DA, Siega-Riz AM. Maternal prepregnancy overweight and obesity and the pattern of labor progression in term nulliparous women. Obstet Gynecol. 2004;104(5 Pt 1):943-951.
11. Reece EA. Perspectives on obesity, pregnancy and birth outcomes in the United States: the scope of the problem. Am J Obstet Gynecol. 2008;198(1):23-27.
12. Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-Related Mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130(2):366-373.
13. Hirshberg A, Srinivas SK. Epidemiology of maternal morbidity and mortality. Seminars in Perinatology. 2017;41(6):332-337. doi:10.1053/j.semperi.2017.07.007
14. Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202(4):335-343.
15. Petersen EE, Davis NL, Goodman D, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths — United States, 2007–2016. MMWR Morbidity and Mortality Weekly Report. 2019;68(35):762-765. doi:10.15585/mmwr.mm6835a3
16. Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension Prevalence and Control Among Adults: United States, 2015-2016. NCHS Data Brief. 2017;(289):1-8.
17. Howell EA. Reducing Disparities in Severe Maternal Morbidity and Mortality. Clin Obstet Gynecol. 2018;61(2):387-399.
18. Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The Black-White disparity in pregnancy-related mortality from 5 conditions: differences in prevalence and case-fatality rates. Am J Public Health. 2007;97(2):247-251.
19. Center for Reproductive Rights. Black Mamas Matter Advancing the Human Right To Safe and Respectful Maternal Health Care.; 2016.
20. Cuschieri S. The STROBE guidelines. Saudi Journal of Anaesthesia. 2019;13(5):31. doi:10.4103/sja.sja_543_18
21. Shah PS, Zao J, Ali S. Maternal Marital Status and Birth Outcomes: A Systematic Review and Meta-Analyses. Maternal and Child Health Journal. 2011;15(7):1097-1109. doi:10.1007/s10995-010-0654-z
22. Shelley-Jones DC, Wein P, Nolan C, Beischer NA. Why do Asian-born women have a higher incidence of gestational diabetes? An analysis of racial differences in body habitus, lipid metabolism and the serum insulin response to an oral glucose load. Aust N Z J Obstet Gynaecol. 1993;33(2):114-118.
23. Chen L, Shi L, Zhang D, Chao SM. Influence of Acculturation on Risk for Gestational Diabetes Among Asian Women. Prev Chronic Dis. 2019;16:E158.
24. Kelly-Weeder S, Cox CL. The impact of lifestyle risk factors on female infertility. Women Health. 2006;44(4):1-23.
25. Yang I, Hall L. Factors related to prenatal smoking among socioeconomically disadvantaged women. Women Health. 2019;59(9):1026-1074.
26. Zhao G, Ford ES, Tsai J, et al. Trends in health-related behavioral risk factors among pregnant women in the United States: 2001-2009. J Womens Health . 2012;21(3):255-263.
27. Robbins C, Boulet SL, Morgan I, et al. Disparities in Preconception Health Indicators - Behavioral Risk Factor Surveillance System, 2013-2015, and Pregnancy Risk Assessment Monitoring System, 2013-2014. MMWR Surveill Summ. 2018;67(1):1-16.
28. Balasch J, Gratacós E. Delayed Childbearing: Effects on Fertility and the Outcome of Pregnancy. Fetal Diagn Ther. 2011;29(4). doi:10.1159/000323142
29. Myers J. Exercise and Cardiovascular Health. Circulation. 2003;107(1). doi:10.1161/01.cir.0000048890.59383.8d
30. CDC. Know Your Risk for Heart Disease | cdc.gov. Centers for Disease Control and Prevention. Published December 10, 2019. Accessed May 23, 2020. https://www.cdc.gov/heartdisease/risk_factors.htm
31. Howard G, Safford MM, Moy CS, et al. Racial Differences in the Incidence of Cardiovascular Risk Factors in Older Black and White Adults. Journal of the American Geriatrics Society. 2017;65(1):83-90. doi:10.1111/jgs.14472
32. Gadson A, Akpovi E, Mehta PK. Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Semin Perinatol. 2017;41(5):308-317.