Laying the Foundation for Quality Improvement: HPV Knowledge and HPV Vaccine Uptake and Attitudes Among Rural Clinic Patients
Adrianna Elbon, OMS-IV, Oklahoma State University for Health Sciences, College of Osteopathic Medicine Rural Medical Track
Krista Schumacher, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Tracy Freudenthaler, PhD, MPH, Northeastern State University
Corresponding Author:Adrianna Elbon, OMS-IV
918-705-1280
Adrianna.f.elbon@okstate.edu
OSU College of Osteopathic Medicine
Disclosures: This work received no external funding support. There are no conflicts of interest to disclose.
Abstract
Background
Despite annual increases in HPV vaccination, uptake rates remain lower than other childhood vaccines while cases of HPV-associated cancers have increased, particularly in rural areas. This study aimed to understand vaccination attitudes among patients at a rural Oklahoma clinic.
Methods
We analyzed data from a survey of parents/caregivers of children aged 9-17 and young adults (YA) aged 18-26 on HPV knowledge, vaccination status, provider recommendation, and reasons for vaccine decision.
Results
The survey yielded 15 YA and 14 caregiver responses. Of YAs, 67% received a vaccine recommendation from a health care provider versus 79% of children. Of these, 80% and 74% respectively had initiated vaccination. Provider recommendation was a top reason for vaccination while “afraid of side effects” was a top reason for refusing vaccination.
Conclusion
Because rural areas lag urban in HPV vaccination, opportunities exist to train rural providers on HPV vaccine messaging to increase rates in these communities.
Keywords: Human papillomavirus, HPV vaccine, vaccine hesitancy, provider recommendation, rural, cancer
Introduction
Each year, it is estimated that there are 14 million new human papillomavirus (HPV) infections in the U.S.1 and 37,000 new cases of HPV-related cancers.2 Vaccination protects against specific strains of HPV and has the potential to prevent more than 90% of all associated cancers (including most cervical, oropharyngeal, anal, penile, vaginal, and vulvar cancers).3 Merck’s Gardasil 9 was approved by the FDA in 2014 and has been the only HPV vaccine available in the U.S. since 2017.4 The vaccine is indicated for use in both females and males 9-45 years of age5 and is more than 99% effective in preventing infection with HPV 16 and 18, two of the most prevalent cancer-causing strains.6
Despite the link between vaccination and cancer prevention, vaccine coverage in the U.S. remains below the Healthy People 2020 goal7 while rates of HPV-associated cancers have increased.8 Moreover, geographic disparities in vaccine coverage have persisted since the first HPV vaccine became available.9 Compared to U.S. urban populations, rural residents have a higher incidence of HPV-related cancer mortality and lower HPV vaccine coverage.10–12 With 93% of counties entirely or partially eligible for federal rural health funding,13 Oklahoma is no different. The state has the highest rate of cervical cancer among all U.S. states as of 2019 (10.3 per 100,000 vs. 7.5 per 100,000 for the nation)14 and one of the lowest rates of up-to-date HPV vaccination for ages 13-17 as of 2021 (56.7% vs. 61.7% for the nation).15
Discrepancies in vaccine uptake in rural areas are multifaceted and can be partly attributed to lack of access to health centers, and influence of poverty.10,12,16 Patient objections and resistance may be based on moral, religious, and cultural beliefs, which may be more prevalent in rural communities.10 Lack of HPV knowledge and HPV literacy12 are also associated with vaccine hesitancy, particularly when it comes to understanding the connection between HPV and cervical cancers.10
The American Academy of Family Physicians (AAFP) urges physicians to strongly recommend the HPV vaccine to their patients.17 While provider recommendation is positively related to vaccine uptake,18–20 research suggests that rural providers may recommend the HPV vaccine at lower rates than their urban counterparts.16,21
Because health care providers and providers-in-training are likely to encounter vaccine hesitancy and objections, understanding patient beliefs and attitudes may be key to shaping stronger vaccine recommendations and increasing uptake. The purpose of this study was twofold: 1) it aimed to examine attitudinal factors related to vaccine decision making among young adult patients and parents/caregivers of vaccine-eligible children at a rural Oklahoma family medicine clinic, and 2) it served as a pilot medical education study to examine the feasibility of conducting a quality improvement (QI) project within the constraints of a four-week clinical rotation.
Methods
An online self-administered Qualtrics survey was used to collect data from eligible respondents: parents/caregivers of children aged 9-17 and young adults aged 18-26 who were patients at a rural Oklahoma family medicine clinic. The survey included five demographic items (age, race, gender, rural/urban residence, education level); five true/false items measuring HPV knowledge (e.g., HPV is rare, males are not affected) adapted from a validated instrument;22 and quantitative items measuring vaccination status, provider recommendation, and check-all items for salient factors in vaccine decision-making (e.g., provider influence, family/friends influence, lack of insurance or vaccine cost, afraid of side effects, or other reason not listed with option to explain).
Potentially eligible participants were recruited by the student on rotation and lead author (AE), who presented information about the study at the end of the patient encounter and provided patients with a study information flyer. No personally identifiable information was collected. The project received approval from the Oklahoma State University Center for Health Sciences Institutional Review Board (IRB). Frequencies were used to analyze data for the target groups.
Results
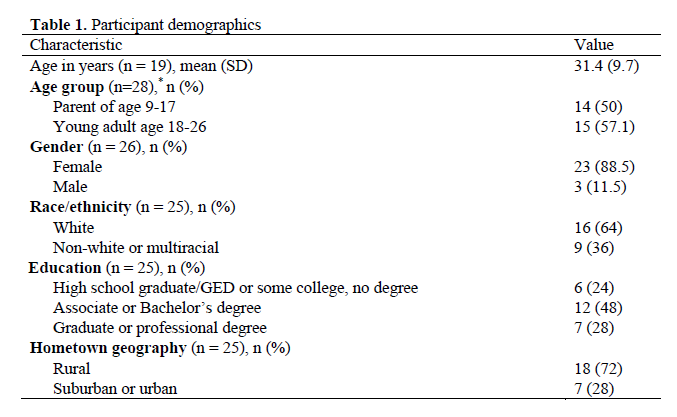
The survey yielded 28 respondents who were primarily white (64%), female (89%), from rural hometowns (72%) and with some college or a college degree (88%) (see Table 1).
HPV knowledge
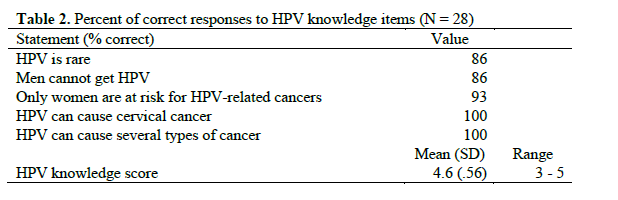
The mean score on HPV knowledge items was 4.6 out of 5, with 86% of respondents correctly answering “HPV is rare” and “Men cannot get HPV,” 93% correctly answering “Only women
are at risk for HPV-related cancers,” and 100% correctly answering “HPV can cause cervical cancer” and “HPV can cause several types of cancer” (see Table 2).
Vaccination status and provider recommendation
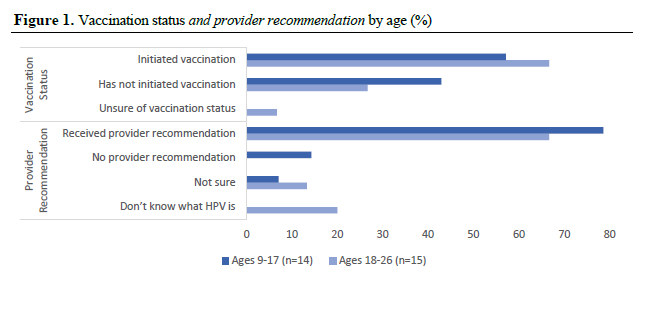
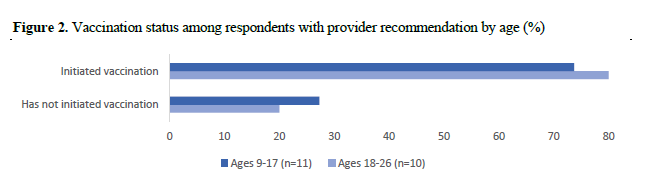
Overall, 57% of children and 67% of young adults had initiated vaccination, and nearly 79% of children and 67% of young adults had received a provider recommendation (see Figure 1). Of those with a recommendation, 74% of children and 80% of young adults had initiated vaccination (see Figure 2).
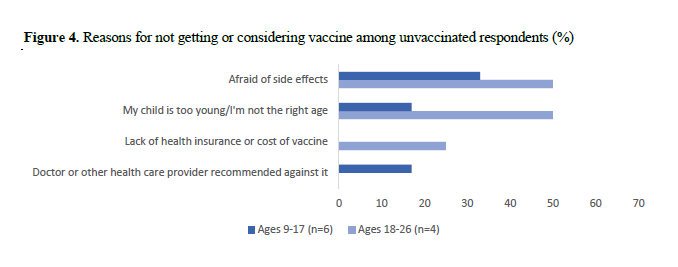
Vaccination decisions
Figure 3 shows reasons given for getting or considering vaccination. Among caregivers of children ages 9-17 (n=12), the top reasons were to protect against HPV infection (58%) and HPV-related cancers (58%) and because a health care provider recommended it (50%). Among young adults (n=12), the top reason was a family or friend recommendation (58%) followed by a health care provider recommendation (50%) and to protect against HPV-related cancers (42%).
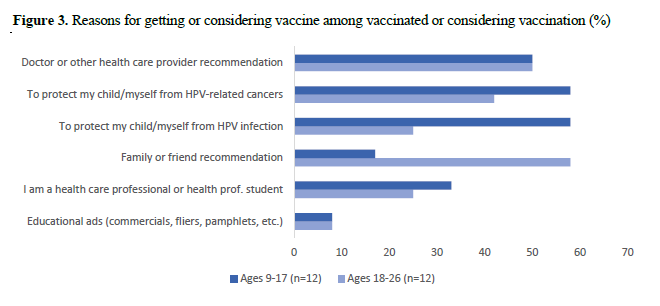
Figure 4 shows reasons given for not getting or considering vaccination. Among caregivers of children ages 9-17 (n=6), the top reason was afraid of side effects (33%) followed by a belief that their child is too young (17%) and a health care provider recommended against vaccination (17%). Among young adults (n=4), the top reasons were afraid of side effects (50%) and a belief that they are not the right age (50%) followed by lack of health insurance or vaccine cost (25%).
Discussion
Vaccine hesitancy is growing problem that providers must face when recommending vaccines. As such, we believe the findings in our paper will appeal to physicians, medical students, residents, and other professionals in the field, especially those working with rural populations. This study shows attitudinal factors are related to vaccine decision-making, even when individuals hold HPV fact-based knowledge. Findings align with the existing literature that health care provider recommendations influence vaccine uptake; however, additional factors and beliefs were found that contribute to the vaccine decision. This is significant because HPV vaccination rates are lower than other childhood vaccines, while HPV-related cancer rates continue to rise, making this a public health concern.
This project was intended to lay the foundation for a QI project to increase HPV vaccination rates at a rural family medicine clinic. The plan for the QI project was designed by the lead author (AE) during the CLME 8122 Early Research Experience (Foundations in QI) course required of all incoming Rural and Tribal Medical Track students. The study discussed in this paper was conducted during a third-year rotation at a rural clinic
Limitations of the study included participant recruitment efforts and limited timeframes to meet admistrative regulations. Participant recruitment was limited by the clinic’s restriction on posting flyers or other study promotion materials. HIPAA regulations would have required submission of a HIPAA waiver to access to patient information to determine eligible participants, but time constraints prevented this approach. These issues led to the small sample size, which consisted of a non-diverse group of respondents. While the project was successful in collecting primary data within a short timeframe, it revealed limitations in conducting research during month-long rotations.
A strength of this study is that it laid the foundation for future QI efforts targeting provider communication with patients to increase HPV vaccine uptake at rural Oklahoma clinics. The clinical implications of the study include the salient factors that emerged that could be useful for health care providers treating young adults and parents/caregivers of eligible children. Both groups indicated that provider recommendation was an important influence in their vaccine decision. This is consistent with literature where health care provider communication directed toward young adults and parents of eligible children is key to vaccination intention and decision-making.23,24 Since young adults cited family or friend recommendations as influential in their vaccination decision, future studies could examine the effectiveness of campaigns that encourage conversations among family and friends regarding vaccination. Finally, while limitations emerged regarding the ability to effectively carry out a survey study during a four-week clinical rotation, the framework exists for future QI studies at residency clinics, which would satisfy ACGME requirements for practice transformation experiences.
All participants in this study correctly identified that HPV is linked to cancer, which the literature indicates is one of several factors related to vaccination.25 However, despite this knowledge, not all survey respondents had chosen to be vaccinated or to have their eligible children vaccinated. This reflects research that indicates HPV knowledge alone does not predict vaccine intention or follow-through,12,26 which underscores the need to examine additional patient beliefs and attitudes. For example, among our survey respondents, two young adults and one caregiver believed they or their child were not the right age for the vaccine. Others were concerned about possible side effects, which has been another cited barrier to vaccination found in the literature.24
Conclusion
QI training prepares medical students for QI experiences in residency and future practice and lays the foundation for viewing health care challenges (e.g., low rates of HPV vaccination) as opportunities for improvement. Noting there is a strong connection between provider recommendation and increased HPV vaccine uptake, there is a need to build provider self-efficacy in making HPV recommendations.27 Similarly, providers-in-training must prepare to respond to patient reluctance and hesitation, which may include overcoming barriers and beliefs. To improve vaccination rates and reduce missed opportunities, providers must talk to parents of eligible children and teens and make strong recommendations.28 Additionally, developing trust with young adult patients and parents of children and teens may be key to positively influencing the vaccine decision.29,30
Acknowledgements
A special thank you to Amanda Hale, DO, adjunct faculty in family medicine for the OSU-COM, for her support of this project.
References
1. Facts about HPV. National Foundation for Infectious Diseases. Published August 29, 2019. Accessed January 31, 2023. https://www.nfid.org/infectious-diseases/facts-about-hpv/
2. How many cancers are linked with HPV each year? Centers for Disease Control and Prevention. Published October 3, 2022. Accessed January 29, 2023. https://www.cdc.gov/cancer/hpv/statistics/cases.htm
3. HINTS Briefs No. 49: HPV and HPV Vaccine Awareness among US Adults. National Cancer Institute Accessed January 29, 2023. https://hints.cancer.gov/docs/Briefs/HINTS_Brief_49.pdf
4. KFF (Kaiser Family Foundation). The HPV vaccine: access and use in the U.S. Women’s Health Policy. Published July 12, 2021. Accessed October 20, 2021. https://www.kff.org/womens-health-policy/fact-sheet/the-hpv-vaccine-access-and-use-in-the-u-s/
5. GARDASIL®9 (Human Papillomavirus 9-valent Vaccine, Recombinant) for Health Care Professionals. MerckVaccines.com. Published 2023. Accessed January 10, 2023. https://www.merckvaccines.com/gardasil9/
6. Oxford Vaccine Group. HPV Vaccine (Human Papillomavirus Vaccine). The University of Oxford. Published January 19, 2022. Accessed January 10, 2023. https://vk.ovg.ox.ac.uk/hpv-vaccine
7. Immunization and Infectious Diseases | Healthy People 2020. Published February 6, 2022. Accessed January 31, 2023. https://wayback.archive-it.org/5774/20220414033335/https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
8. Liao CI, Francoeur AA, Kapp DS, Caesar MAP, Huh WK, Chan JK. Trends in human papillomavirus–associated cancers, demographic characteristics, and vaccinations in the US, 2001-2017. JAMA Network Open. 2022;5(3):e222530. doi:10.1001/jamanetworkopen.2022.2530
9. Hirth J. Disparities in HPV vaccination rates and HPV prevalence in the United States: a review of the literature. Hum Vaccin Immunother. 2019;15(1):146-155. doi:10.1080/21645515.2018.1512453
10. Vanderpool RC, Stradtman LR, Brandt HM. Policy opportunities to increase HPV vaccination in rural communities. Hum Vaccin Immunother. 2019;15(7-8):1527-1532. doi:10.1080/21645515.2018.1553475
11. Peterson CE, Silva A, Holt HK, Balanean A, Goben AH, Dykens JA. Barriers and facilitators to HPV vaccine uptake among US rural populations: A scoping review. Cancer Causes Control. 2020;31(9):801-814. doi:10.1007/s10552-020-01323-y
12. Mohammed KA, Subramaniam DS, Geneus CJ, et al. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39-43. doi:10.1016/j.ypmed.2018.01.016
13. Rural Health Grants Eligibility Analyzer. Health Resources & Services Administration. Published n.d. Accessed February 7, 2023. https://data.hrsa.gov/tools/rural-health?tab=StateCounty
14. Cancer statistics at a glance. United States Cancer Statistics: Data Visualizations. Published 2022. Accessed January 31, 2023. https://gis.cdc.gov/grasp/USCS/DataViz.html
15. Centers for Disease Control and Prevention. Vaccination coverage among adolescents (13-17 years). TeenVaxView. Published 2021. Accessed January 31, 2023. https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/data-reports/index.html
16. Goessl CL, Christianson B, Hanson KE, et al. Human papillomavirus vaccine beliefs and practice characteristics in rural and urban adolescent care providers. BMC Public Health. 2022;22(1):1322. doi:10.1186/s12889-022-13751-3
17. Immunization schedules | Red Book Online | AAP Point-of-Care-Solutions. American Academy of Pediatrics. Published 2021. Accessed January 24, 2023. https://redbook.solutions.aap.org/selfserve/ssPage.aspx?SelfServeContentId=Immunization_Schedules
18. Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: a meta-analysis and systematic review. Prev Med. 2021;148:106554. doi:10.1016/j.ypmed.2021.106554
19. Caldwell AC, Madden CA, Thompson DM, et al. The impact of provider recommendation on human papillomavirus vaccine and other adolescent vaccines. Hum Vaccin Immunother. 2021;17(4):1059-1067. doi:10.1080/21645515.2020.1817713
20. Freudenthaler T, Elbon A, Schumacher K. Understanding how health care provider recommendations and messaging strategies influence HPV vaccine uptake: A study of undergraduate student perspectives. Oklahoma State Medical Proceedings. 2021;5(2). https://okstatemedicalproceedings.com/index.php/OSMP/article/view/158
21. Bhatta MP, Phillips L. Human papillomavirus vaccine awareness, uptake, and parental and health care provider communication among 11- to 18-year-old adolescents in a rural Appalachian Ohio county in the United States. The Journal of Rural Health. 2015;31(1):67-75. doi:10.1111/jrh.12079
22. Waller J, Ostini R, Marlow LAV, McCaffery K, Zimet G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev Med. 2013;56(1):35-40. doi:10.1016/j.ypmed.2012.10.028
23. Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19-26: Importance of a physician’s recommendation. Vaccine. 2011;29(5):890-895. doi:10.1016/j.vaccine.2009.12.063
24. Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Preventive Medicine. 2013;57(5):414-418. doi:10.1016/j.ypmed.2013.05.013
25. Wilson AR, Hashibe M, Bodson J, et al. Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: an observational study. BMC Women’s Health. 2016;16(1):41. doi:10.1186/s12905-016-0323-5
26. Ratanasiripong NT. Factors related to human papillomavirus (HPV) vaccination in college men. Public Health Nurs. 2015;32(6):645-653. doi:10.1111/phn.12198
27. McRee AL, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: Findings from a statewide survey of healthcare providers. J Pediatr Health Care. 2014;28(6):541-549. doi:10.1016/j.pedhc.2014.05.003
28. Smith PJ, Stokley S, Bednarczyk RA, Orenstein WA, Omer SB. HPV vaccination coverage of teen girls: The influence of health care providers. Vaccine. 2016;34(13):1604-1610. doi:10.1016/j.vaccine.2016.01.061
29. MacArthur KR. Beyond health beliefs: The role of trust in the HPV vaccine decision-making process among American college students. Health Sociology Review. 2017;26(3):321-338. doi:10.1080/14461242.2017.1381035
30. Nan X, Daily K, Richards A, et al. The role of trust in health information from medical authorities in accepting the HPV vaccine among African American parents. Hum Vaccin Immunother. 2018;15(7-8):1723-1731. doi:10.1080/21645515.2018.1540825
31. LeRoy G, Fincher J, Phipps MG, Donovan D. Give a confident, clear, and consistent recommendation for HPV vaccine to increase uptake! Published online February 3, 2021. Accessed October 22, 2021. https://www.immunize.org/letter/recommend_hpv_vaccination.pdf