Breastfeeding and Native American Women’s Preference in Food Taste
Liza-Ann Suba, M.S., Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Hope Davis, B.S., Office of Medical Student Research, Oklahoma State University Center for Health Sciences, Tulsa, Oklahoma
Kristen McPherson, M.P.H., Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Allison Garnett, D.O. Department of Obstetrics and Gynecology, Oklahoma State University Center for Health Sciences, Tulsa, Oklahoma
Alexis B Jones, Ph.D. Oklahoma State University Center for Health Sciences, Department Pharmacology and Physiology, Tulsa, Oklahoma
Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, Oklahoma
Corresponding Author: Liza-Ann Suba, Oklahoma State University Center for Health Sciences
Address: 1111 W 17th St., Tulsa, OK 74107, United States.
Email: liza.whitaker@okstate.edu Phone: (405) 816-0413
Funding: This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Abstract:
Background:
To ascertain whether breastfeeding influences Native American women’s interest in eating specific food tastes, women were surveyed upon arrival to their 6-week postpartum appointment to assess interest in eating foods from 5 different taste categories.
Methods:
Surveys were offered at check in, and no identifying information (name, age, race, SSN) or protected health information was collected. Women were asked whether they were breastfeeding, number of infants delivered, and if this was their first baby. Level of hunger was rated on a Likert scale that ranged from 1 (not hungry at all) to 9 (very hungry), with 5 indicating “don’t care.”
Results:
Overall, breastfeeding women did indicate a significant difference in eating specific foods from within the sweet taste category when compared to non-breastfeeding women. Non-breastfeeding women demonstrated a significant positive correlation between hunger scores and their inclination to consume chocolate bars, whereas breastfeeding women exhibited greater interest in consuming chocolate bars overall. Lastly, there were no significant differences between breastfeeding and non-breastfeeding women when it came to preferences in eating foods within the other taste groups (salty, bitter, sour, meaty, and hot).
Conclusion:
These findings represent the first approach at assessing the potential influence of breastfeeding within the Native American population on the level of interest for eating certain foods. These findings may provide a starting point for examining food preferences within a subset of the Native American population with the hopes of further evaluating potential cultural influences in future studies.
Introduction
During pregnancy, mothers are known to experience food cravings. However, there has not been much research into why these cravings develop.1 Studies of the dopaminergic reward circuits in the brain have uncovered speculated links of consuming palatable foods to be as addicting as using substances of abuse, such as alcohol or nicotine.2 Moreover, food cravings and aversions can potentially be correlated to the hormonal and physical changes experienced during pregnancy and the postpartum period.3 Some women that are experiencing cravings combine foods from different taste categories, such as pickles and ice cream, while others may have the urge to eat non-food items, a disorder known as pica.4 Furthermore, research has shown that some food cravings, such as for unpasteurized dairy products or fish with potentially high mercury content, can lead to adverse effects on fetal development.5 Increased intake of foods with a high glycemic index during pregnancy may lead to excessive weight gain and other antepartum complications, such as gestational diabetes. A review of literature focusing on the impact of maternal high fat diets, during gestation and lactation, reveal potential adverse outcomes in offspring regarding their brain development, behavioral changes, and hypercholesterolemia.6 A study published by Duffy et al. in 1998 is the only longitudinal study to examine taste preferences in a cohort of women before and during the entirety of their pregnancy. This study found that pregnant women report a decrease in intensity ratings of salt and bitter during the second and third trimesters, leading researchers to postulate that this may lead to cravings for foods such as pickles.7 There is inconsistency in findings from studies into this topic. Findings from some studies show no change in pregnant and postpartum women’s sweet and sour taste, while some indicate that sweet taste may increase during the first trimester of pregnancy.8 Brown et al. found that pregnant women in their study were unable to correctly identify the difference in salt concentrations in samples when compared to nonpregnant women, suggesting a physiologic mechanism to promoting increased salt intake during pregnancy.9
While much of the focus on maternal health, research, and education is during pregnancy and childbirth, the postpartum period deserves attention as well. Improved quality of care during the postpartum period has the potential to improve maternal and neonatal health outcomes and overall well-being. The American College of Obstetricians and Gynecologists (ACOG) recommends an initial assessment within the first 3 weeks postpartum, as well as ongoing care as needed and a comprehensive well-woman visit no later than 12 weeks after birth.10 Postpartum care should address components such as reproductive plans and contraception options, pregnancy complications, mental health, postpartum problems, and infant feeding plan, among others.10 For women who are breastfeeding, this is an important component that should be discussed. While breastfeeding is physically demanding and is associated with increased energy and metabolic requirements, it is associated with many maternal and neonatal benefits. Studies have also shown that breastfeeding may improve maternal-infant bonding.11 Little research has been conducted regarding taste perception and preferences in breastfeeding women. In 2019, a study investigating whether breastfeeding altered food preferences between native English-speaking women and Spanish-speaking women was conducted by Solis et al.12 Other than this one article, to our knowledge, there have been no other studies conducted regarding taste perception and taste preference in breastfeeding women. This is especially true overall for Native American populations, where there has been little research done within the population. While attempting to find research articles relating to this topic, phrases such as “food preferences during breastfeeding,” “maternal food preferences,” and “breastfeeding and food tastes” were utilized. Majority of the articles retrieved focused on how the act of breastfeeding influenced nutrition and the overall development of infants and children. Physiological changes of hormones, electrolyte balances, and fluid volume during pregnancy have been previously studied to better understand women’s health and how to keep a woman healthy during pregnancy. Taking this a step further and following up during lactation, there is a potential to observe what physiological changes may occur postpartum. Better understanding of the influences on maternal food choices during the postpartum period provides insight on the food choices for the entire household including maternal offspring.
With this in mind, the aim of our study focused on examining whether breastfeeding influenced the food preferences in a population of Native American women who are part of the Cherokee Nation tribe in Tahlequah, Oklahoma during their 6-week postpartum appointment. We chose to study women in the Native American demographic due to a lack of previous research within this population. Native women were surveyed and asked to indicate their interest in eating various foods that were representative of classic taste categories (sweet, hot, meaty, salty, etc). Participants were then asked what taste category influenced their interest in eating any of the foods listed. The focus of this study was to compare food interests and taste preferences in Native American mothers primarily of the Cherokee Nation population who designated themselves as breastfeeding and those who did not (see Demographics and Procedures, below). Furthermore, this provided insight on the possibility of a potential role of cultural and ethnic influences on eating certain foods, as our findings may be compared to the findings in the prior study completed by Solaris et al. This study serves as a baseline for comparison as it utilized the same survey to investigate the taste preferences in both Spanish-speaking and English-speaking participants. Although the original survey was created to investigate food preferences between Spanish- and English-speaking respondents, many of these foods can be historically tied to Native American cuisine following colonization. Examples include tomatoes, fish, other meats, and peppers; etc. therefore it was deemed acceptable to reuse Solaris et al.’s original survey with this study’s population.13
Methods
Demographics and procedures
We surveyed Native American women utilizing the Women’s Clinic at W.W. Hastings Indian Hospital, a health facility owned by the Cherokee Nation and located in Tahlequah, Oklahoma. Cherokee Nation Health Services is a multifaceted health care system and the largest tribally-operated health care system in the United States.14 The patient’s served at this facility are either required to have a Certificate Degree of Indian Blood (CDIB) card, or be the biological mother who had given birth to an infant of Native American heritage. Although tribal citizens from all over the United States travel to receive a variety of services, Cherokee Nation is the largest tribe in the United States, with over 450,000 citizens globally.15 Participants for this study were recruited as they checked in at the reception desk for their 6-week postpartum appointment. Mothers were informed that participation was voluntary and required filling out a survey in the waiting room prior to their appointment. Upon completion, surveys were sealed in provided envelopes and stored confidentially in the clinic until collection.
Taste Interest Survey
Instructions at the beginning of the provided survey discussed the purpose of this study and identified the supporting organization. It was explained that survey completion was optional and would be considered consent to participate in this study. Additionally, it was requested that respondents not include any identifying information (name, age, address, social security number, etc.) or other protected health information when completing the survey. Study participants were asked if this was their first baby, number of infants born, and if they were breastfeeding. Next, the current hunger level of respondents was determined using a Likert scale. This was done in order to minimize differences in responses based on the time of survey participants’ most recent meal. This scale ranged from 1 (“Not at all hungry”) to 9 (“Very hungry”). The next portion of the survey contained a list of specific foods, of which participants were instructed to rate their interest in eating. A Likert scale was again used for this, ranging from 1 (“Really don’t want to eat that food”) to 9 (“Really do want to eat that food”). This food interest survey was initially created by colleagues within our organization, inspired by a survey developed by Pereira-Derderian (D.T.B. Pereira-Derderian, unpublished observations), and utilized in a similar study with a different patient demographic.12 The foods selected for the survey list were chosen to represent general taste categories (salt, sweet, sour, hot, meaty). On the last page of the survey, participants were asked to reflect on the foods they rated a 9 and indicate if they would eat those foods at that moment. Based on this decision, women were asked what food tastes influenced their interest in eating the highly rated foods (salty taste, sweet taste, etc.). Lastly, it was asked if any of the food items rated 7-9 were eaten in the last 2-3 days. If so, participants were asked to specify which foods and if not, they were asked to indicate why not. The survey and protocols were reviewed by the Oklahoma State University – Center for Health Sciences Institutional Review Board and determined to meet exempted criteria under federal guidelines (21 CFR 56.108(b) (3)).
Demographic data
The number of breastfeeding and non-breastfeeding respondents for whom this was their first baby vs. those for whom it was not their first baby, as well as numbers for whom it was a multiple birth or a single birth, was collected and is represented in Table 1.
Food Interest Data Analyses and Statistics
Data are shown as means ± s.e.m. Significance was set at p < .05.
Ratings of interest in eating various foods within each taste category (salty, sweet, sour, bitter, hot) were analyzed using separate 3-way repeated measures (rm) Analysis of Variance (ANOVA) with breastfeeding (yes or no) and specific foods as factors, repeated for foods. In addition, average scores for each taste category (salty, sweet, sour, bitter, hot) were calculated for each Native woman, and ratings of interest in eating foods across these categories then were analyzed using 3-way rm. ANOVA with breastfeeding (yes or no), and taste category as factors, repeated for taste category. Hunger ratings were analyzed using 2-way ANOVA with breastfeeding (yes or no) as factors. Statistically significant main effects or interactions identified by ANOVAs were further analyzed using Fisher's LSD tests; effect sizes are shown as partial eta2 (pƞ2).
Regression analyses were performed on the relationship between hunger and interest in eating foods in women who were or were not breastfeeding for each of the taste categories.
Results
Demographic data
Fifty-five surveys were collected and all data collected was included in analyses. Forty-one respondents indicated that they were breastfeeding their infant and 14 reported they were not breastfeeding; additionally, comparison of hunger rating reported at the time of survey completion is represented in Table 1. For the majority of both breastfeeding and non-breastfeeding respondents, this was not their first baby (Table 1).
Food Interest Data
Two-way, repeated measures ANOVA on food taste categories revealed no main effects of breastfeeding status on interest score [F(df1,df2)=1.098, p=0.329], no main effect of food category on interest score [F(df1,df2)=0.371, p=0.832], and no interaction between breastfeeding status and food category on interest score [F(df1,df2)=1.267, p=0.306) (Figure 1). Breastfeeding women reported no differences in hunger compared to non-breastfeeding women (Table 1).
Breastfeeding status did not significantly alter interest in eating foods in any taste category; however, breastfeeding women tended to be more interested in eating sweet foods than non-breastfeeding women. (Figure 1). The number of breastfeeding and non-breastfeeding respondents and their responses to whether they had eaten any of the foods they indicated as being of interest during the preceding 2-3 days was also reported (Table 2).
Interest in eating specific foods within each taste category (salty, sweet, sour, bitter, meaty, hot) was reported by respondents who were breastfeeding and who were not breast-feeding, represented in Table 3. Analyses of interest in eating foods within specific taste categories using 2-way, repeated measures ANOVA revealed no differences in any category (Table 3). However, within the sweet category, there were differences in specific foods (see Table 3).
Women who breastfeed their infants were found to be significantly more interested in eating chocolate bars within the sweet taste category compared to non-breastfeeding women (p<0.05) (Figure 2). In contrast, the relationship between hunger and interest in eating chocolate bars was more tightly linked in non-breastfeeding women (p<0.05) (Figure 3). However, the other specific foods within the sweet taste category were comparable in interest between breastfeeding and non-breastfeeding Native women. (Figure 2).
Relationship between hunger scores and interest in eating chocolate bars was then investigated (Figure 3). Regression analyses of hunger scores reported at the time the survey was taken (x-axes) and interest in eating chocolate bars (y-axes) in women who were breastfeeding and non-breastfeeding (Figure 3). There was a significant positive relationship between hunger and interest in eating chocolate bars in women who were not breastfeeding (p<0.05), but not in women who were breastfeeding (Figure 3).
Table 1 Parity, Lactation, and Hunger Ratin
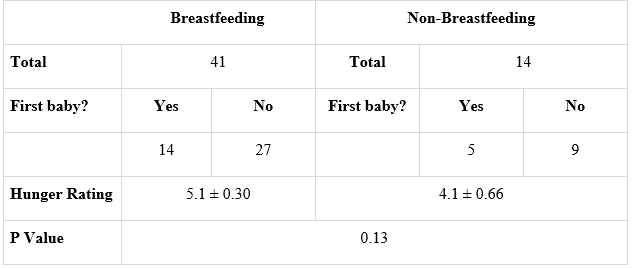
Number of Native American women respondents who reported whether they were breastfeeding or that they were not breastfeeding and whether or not this was their first baby. Comparison of hunger rating reported at the time of survey completion. Number of breastfeeding and non-breastfeeding respondents and their response to a question “How hungry are you right now?” on a scale of 1 (“not hungry at all”) to 9 (“very hungry”).
Figure 1. Averages of food category interest. Interest in eating foods of each food category in non-breastfeeding (blue bars) and breastfeeding respondents (orange bars).
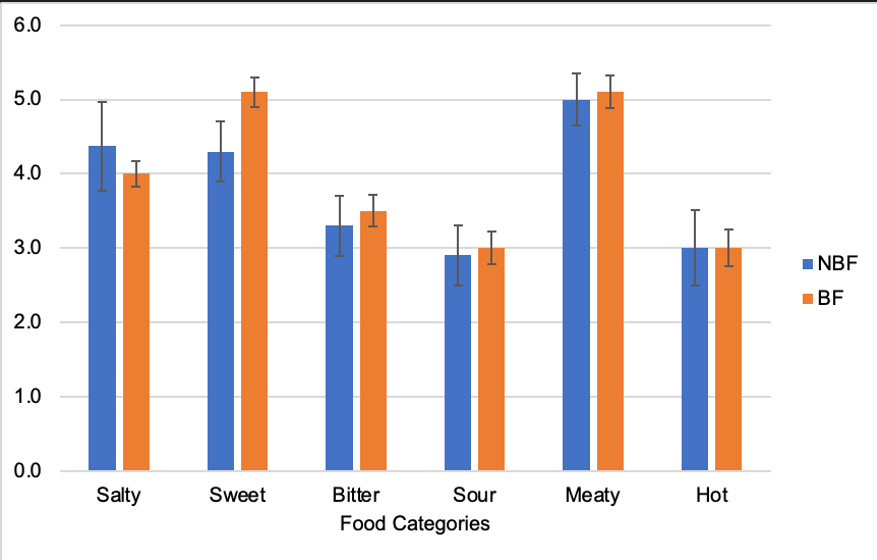
Figure 2. Interest in eating specific foods in the sweet category in non-breastfeeding (blue bars) and breastfeeding respondents (orange bars).
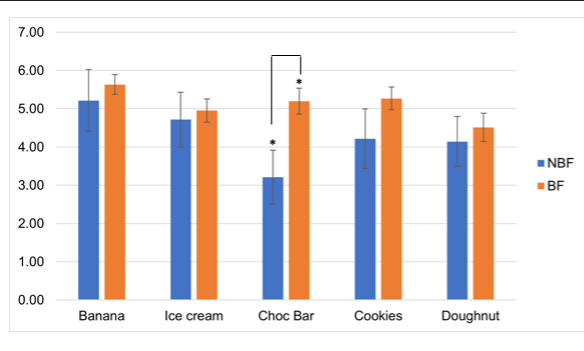
Figure 3. Relationship between hunger scores and interest in eating chocolate bars.
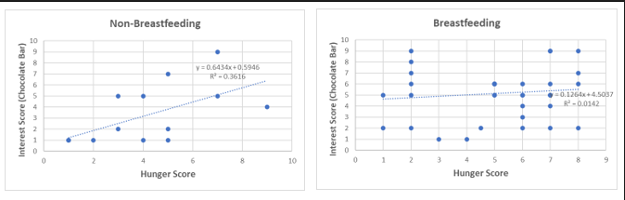
Table 2. Consumption of Indicated Foods of Interest
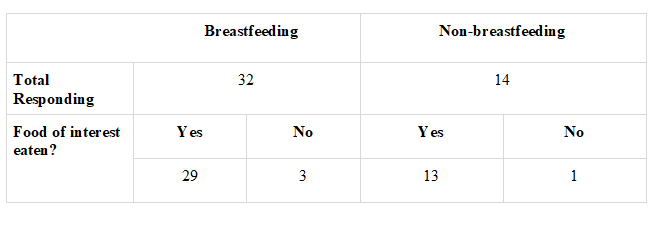
Number of breastfeeding and non-breastfeeding respondents and their responses to whether they had eaten any of the foods they indicated as being of interest during the preceding 2-3 days.
Table 3 Interest scores for specific foods within taste categories.
|
Breastfeeding |
Non-Breastfeeding |
| Salty |
|
|
| Potato chips |
4.0 |
4.1 |
| Pretzels |
3.0 |
3.7 |
| Nachos |
5.1 |
4.1 |
| Nuts |
5.1 |
5.3 |
| Popcorn |
2.9 |
4.6 |
| Sweet |
|
|
| Banana |
5.6 |
5.2 |
| Ice Cream |
5.0 |
4.7 |
| Chocolate Bar |
5.2 |
3.2 |
| Cookies |
5.3 |
4.2 |
| Donuts |
4.5 |
4.1 |
| Sour |
|
|
| Sauerkraut |
1.8 |
1.6 |
| Pickles |
4.8 |
4.7 |
| Lemon/Lime |
3.2 |
3.8 |
| Grapefruit |
2.0 |
1.8 |
| Bitter |
|
|
| Broccoli |
4.3 |
4.5 |
| Cauliflower |
2.8 |
2.1 |
| Cucumbers |
4.3 |
5.0 |
| Celery |
3.3 |
2.6 |
| Greens |
2.7 |
2.0 |
| Tomatoes |
3.5 |
3.6 |
| Meaty |
|
|
| Tuna |
2.4 |
1.7 |
| Hamburger |
6.4 |
6.9 |
| Pork chop |
5.3 |
4.4 |
| Steak |
6.4 |
7.1 |
| Fried chicken |
4.9 |
4.9 |
| Hot |
3.0 |
3.9 |
| Hot Wings |
3.0 |
3.9 |
Jalapeno Pepper |
3.0 |
2.1 |
Interest in eating various foods within taste categories (salty, sweet, sour, bitter, meaty, hot) reported by respondents who were breastfeeding and who were not breast-feeding.
Discussion
This study was adapted from a similar study based out of a clinic in Tulsa, Oklahoma comparing breastfeeding and non-breastfeeding mothers who spoke primarily English or Spanish. To our knowledge, this is the only other study examining the potential influence of breastfeeding on a woman’s food preferences. We adapted this work by reusing the original survey, written in English, to address this topic in Native American women, specifically those being served by Cherokee Nation Health Services in Tahlequah, Oklahoma. This adaptation may serve as a potential starting point for future research and the collection of information aimed at better understanding the food choices of Native American women during the postpartum period. The insights gathered from this type of work can guide health recommendations for this specific population in the future.
Examination of our data revealed that the majority of our study participants were breastfeeding mothers, regardless of whether this was the mother’s first child or not. This may be due to home influences, provider recommendations for breastfeeding, or other factors not explored in the survey. Additionally, hunger ratings tended to be higher among Native American respondents who reported to be breastfeeding their infant, even though there was no statistical significance noted (Table 1). In the Solaris et. al study, participants across both language groups reported comparable hunger ratings, regardless of breastfeeding status and the time of day in which they completed their survey.12 Our findings seem to correlate with the advised increase in caloric requirements for breastmilk production and maintaining lactation, as women who breastfeed require as many as 500 additional kcal/day in addition to the normal requirements for non-pregnant women.16 Moreover, no remarkable differences were observed in the preferences for foods within the various taste categories between the two study groups, with the exception of the sweet taste category (Figure 1). Compared with non-breastfeeding Native American women, women who were breastfeeding were significantly more interested in eating chocolate bars (p<0.05) (Figure 2). While breastfeeding women were more interested in eating chocolate bars, non-breastfeeding women showed a significant positive correlation between hunger scores and interest in eating chocolate bars compared to breastfeeding women (Figure 3). In the original study per Solaris et. al, there was noted interaction between the primary language of study participants and the specific foods within each category. The authors found that English respondents had a higher interest in eating ice cream, whereas Spanish respondents had the greatest interest in eating bananas and cookies with both items being significantly greater than their interest in eating chocolate bars.12 Thus, there was a difference observed in preferences for different foods within the sweet category between the Spanish and English respondents in the original study and when compared to the Native American participants from our study, we see that there is also a difference observed in the preference for the specific foods within the sweet category. While there are a number of factors that could have influenced these differences, it could be considered that there may be a cultural influence present.
Previous research has noted that food tastes reach as far back into the prenatal period with the activation of taste buds starts around the 30th week of gestation as the amniotic fluid’s composition varies based on material diet.17 Although our study focuses primarily on mothers in the postpartum period, the flavor profiles and food choices that she makes during pregnancy and following birth may have longitudinal effects. Exposure to flavor profiles during the antepartum period, (breast vs bottle) milk, and during the transition to solid foods can influence a child’s food preference profile.18 It is also important to consider social factors such as the availability of food groups and the phenomena of food deserts when analyzing food choices within a population. Thus, the development of an individual’s preferences for particular foods and taste categories involves motivational, behavioral, and genetic aspects. Considering these ideals, it can be postulated that the development of taste preferences is multifactorial and related to factors such as socioeconomic status, availability of diverse food profiles, and overall the lifestyle of a mother during the postpartum period. Developing survey questions specific to these components can provide better insight on reported hunger levels (Table 1) and interest in certain sweet foods among breastfeeding women (Figure 2) emphasizes the importance of encouraging postpartum women to eat a balanced and nutritional diet in order to maintain energy and metabolic demands, as well as improve maternal health outcomes. Patient education on this topic has the potential to reduce the incidence of cardiovascular disease (CVD), the leading cause of death in women.19
Limitations of our study include inability to conduct certain statistical analyses due to presence of only two study groups, as well as a relatively small sample size. As stated previously, conducting research studies within a Native American population is unique, and to our knowledge, no studies in this population have been conducted of this design. Adjustment of our survey to include more cultural and traditional food options for this population could also increase the applicability of our study. Additionally, including an equal number of specific foods in each food category may decrease feelings of choice overload during survey completion. The study may also be modified to take into consideration time of day in which the survey is administered. This could be done by standardizing the time of day in which it is administered along with ensuring that the foods on the survey are appropriate for interest in consumption during that specific time of day. The survey may also be modified to expand questioning on when the last time the mothers ate as well as what was eaten in order to provide more insight into the data.
Furthermore, additional studies with more than 55 participants can provide a more robust representation of the potential influence of breastfeeding on food choices during the postpartum period. Future studies including additional survey responses will provide enough data to perform statistical analysis, and further insight to examine interest in specific foods from the various taste categories. However, these findings provide the initial steps in better understanding how breastfeeding may affect food preferences in Native American women and their food choices. This is important because maternal food choices can have implications on the overall health of a mother and her offspring. This includes maternal health issues such as postpartum weight loss and postpartum nutritional deficiencies. It also includes childhood obesity since maternal food preferences may influence family meal decisions.
References
1. Bayley TM, Dye L, Jones S, DeBono M, Hill AJ. Food cravings and aversions during pregnancy: relationships with nausea and vomiting. Appetite. 2002;38(1):45-51. doi:10.1006/appe.2002.0470
2. Alonso-Alonso M, Woods SC, Pelchat M, et al. Food reward system: current perspectives and future research needs. Nutr Rev. 2015;73(5):296-307. doi:10.1093/nutrit/nuv002
3. Hill AJ, Cairnduff V, McCance DR. Nutritional and clinical associations of food cravings in pregnancy. J Hum Nutr Diet. 2016;29(3):281-289. doi:10.1111/jhn.12333
4. Aparna PV, Austin RD, Mathew P. PICA. Indian J Dent Res. 2012;23(3):426-427. doi:10.4103/0970-9290.102246
5. Tam C, Erebara A, Einarson A. Food-borne illnesses during pregnancy: prevention and treatment. Can Fam Physician. 2010;56(4):341-343. https://www.ncbi.nlm.nih.gov/pubmed/20393091
6. Gawlińska K, Gawliński D, Filip M, Przegaliński E. Relationship of maternal high-fat diet during pregnancy and lactation to offspring health. Nutr Rev. 2021;79(6):709-725. doi:10.1093/nutrit/nuaa020
7. Duffy VB, Bartoshuk LM, Striegel-Moore R, Rodin J. Taste changes across pregnancy. Ann N Y Acad Sci. 1998;855:805-809. doi:10.1111/j.1749-6632.1998.tb10663.x
8. Choo E, Dando R. The Impact of Pregnancy on Taste Function. Chem Senses. 2017;42(4):279-286. doi:10.1093/chemse/bjx005
9. Brown JE, Toma RB. Taste changes during pregnancy. Am J Clin Nutr. 1986;43(3):414-418. doi:10.1093/ajcn/43.3.414
10. Optimizing postpartum care. Accessed April 20, 2023. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/05/optimizing-postpartum-care
11. Liu J, Leung P, Yang A. Breastfeeding and active bonding protects against children’s internalizing behavior problems. Nutrients. 2013;6(1):76-89. doi:10.3390/nu6010076
12. Solis LV, Bowes AL, Vazquez-Sanroman D, Curtis KS. Breastfeeding and women’s interest in specific food tastes. Physiol Behav. 2019;208:112566. doi:10.1016/j.physbeh.2019.112566
13. Park S, Hongu N, Daily JW. Native American foods: History, culture, and influence on modern diets. Journal of Ethnic Foods. 2016;3(3):171-177. doi:
14. Health services. Cherokee Nation Health Services. Accessed June 19, 2023.
15. Cherokee Nation home: Cherokee Nation Website. Accessed July 27, 2023.
16. Kominiarek MA, Rajan P. Nutrition Recommendations in Pregnancy and Lactation. Med Clin North Am. 2016;100(6):1199-1215. doi:
17. Paglia L. Taste development and prenatal prevention. Eur J Paediatr Dent. 2019;20(4):257. doi:
18. Sina E, Buck C, Jilani H, et al. Association of Infant Feeding Patterns with Taste Preferences in European Children and Adolescents: A Retrospective Latent Profile Analysis. Nutrients. 2019;11(5). doi:
19. Graves M, Howse K, Pudwell J, Smith GN. Pregnancy-related cardiovascular risk indicators: Primary care approach to postpartum management and prevention of future disease. Can Fam Physician. 2019;65(12):883-889. https://www.ncbi.nlm.nih.gov/pubmed/31831487
Author’s Contact Information
Liza-Ann Suba: liza.whitaker@okstate.edu
Hope Davis: hope.davis11@okstate.edu
Kristen McPherson: kristen.mcpherson@okstate.edu
Allison Garnett, DO: allison.garnett@okstate.edu
Alexis Jones, PhD: alexis.jones@okstate.edu