Statin Guidelines: The Past, The Present, and The Future
Steve Dixon, D.O, M.P.H, Lauren Devine, Pharm D, & Steve Kim, D.O.
ABSTRACT
In June of 2013, the American College of Cardiology and American Heart Association released a revised version of guidelines regarding the recommendation of HMG CoA reductase inhibitors (statins). Following this, the United States Preventive Services Task Force released its own set of guidelines regarding the use of statins in 2016. Both sets of guidelines included recommendations that differed significantly from previously established statin recommendations. However, the guidelines included several differences between the two sets. This article discusses both sets of guidelines and reviews the published literature analyzing the adoption of the new recommendations.
INTRODUCTION
In May of 2001, the National Heart, Lung, and Blood Institute (NHLBI) published the Adult Treatment Panel’s
third addition of guidelines for the identification, evaluation, and treatment of patients with elevated cholesterol.
These guidelines essentially focused on titrating lipid therapy based on target LDL-C and non-HDL-C levels. After this publication,
the NHLBI reconvened expert panels in 2008 to update the guidelines based on systematic evidence-based reviews. Prior to the release
of this update, in 2011 the Institute of Medicine released two reports containing recommendations for developing systematic evidence-based
reviews and establishing clinical guidelines. With the release of these new guidelines, the NHLBI partnered with the American College of
Cardiology (ACC), American Heart Association (AHA), and other societies in June of 2013 to form an expert panel. The task of the panel was
to reevaluate the previously published lipid guidelines using data from randomized control trials.¹
The expert panel was asked to provide new guideline recommendations for treating cholesterol levels in an attempt to lower atherosclerotic cardiovascular disease (ASCVD) risk. ASCVD was defined as stroke, coronary artery disease, or peripheral arterial disease. The expert panel was focused on reviewing data that could be used to identify those patients most likely to benefit from therapy and to design guidelines that would be simple to implement in the clinical setting.¹
Several strategies had been previously used to lower the risk of ASCVD, including treating to target cholesterol level, lowest possible cholesterol level, and various risk-based models. However, the expert panel was unable to find any randomized control trials to justify the use of these methods, and several target levels within dosage titration models failed to account for the potential adverse effects of treatment. In review of the published randomized control trials available, the expert panel was only able to identify the use of fixed dosages of lipid lowering medications as a treatment strategy. Therefore, the panel could not support the previously released lipid guidelines.¹
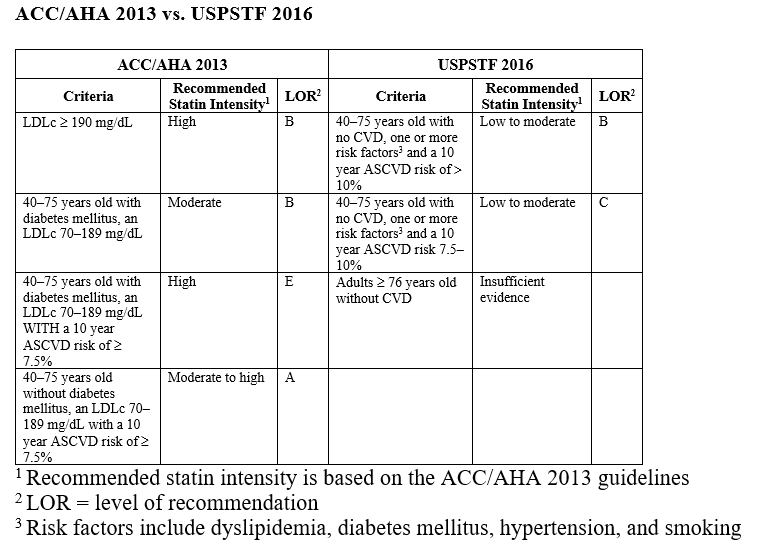
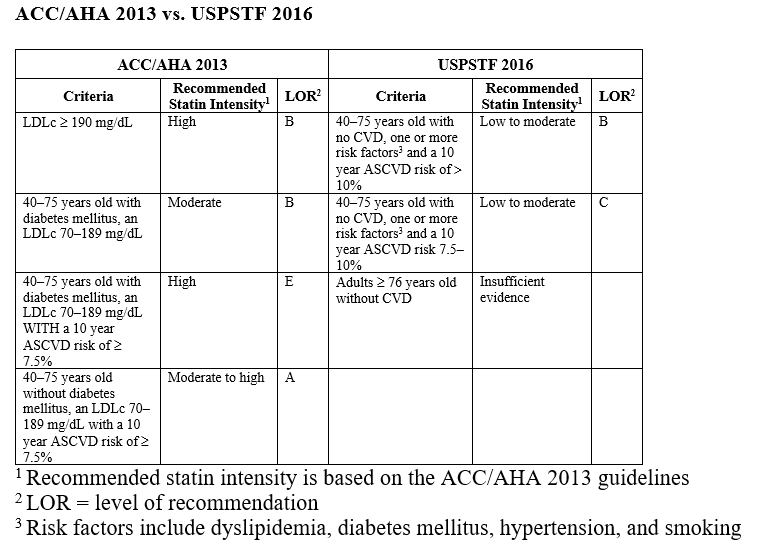
In November of 2013, the ACC/AHA Expert Panel released a new version of recommendations for treating cholesterol to reduce ASCVD risk. Apart from prioritizing lifestyle modification with diet and exercise, the new recommendations focused on four groups in which evidence suggested the benefit of therapy with statins plainly offset the risk of use. These groups are as follows:
1. Individuals with clinical ASCVD, as defined as previous coronary syndrome, angina, history of stroke, or peripheral arterial disease.
2. Individuals with primary elevations of LDL-C greater than 190mg/dL
3. Individuals with diabetes aged 40 to 75 with LDL-C between 70 and 189mg/dL and without clinical ASCVD
4. Individuals without clinical ASCVD or diabetes with LDL-C between 70 and 189mg/dL and an estimated ASCVD risk score of ≥ 7.5%.
The ASCVD score was based off data from pooled cohorts to provide a 10-year risk for an individual’s likelihood of developing an atherosclerotic disease process or event. Factors included in the scoring calculation included age, gender, HDL-C, systolic blood pressure, treatment of blood pressure, smoking status, and diabetic status.¹
Treatment of patients with clinical ASCVD were subdivided into those over 75 years old and those under 75 years old. For patients under 75 years old, high-intensity statin therapy was recommended, while for those over 75 years of age, moderate-intensity statin was recommended if the patient could not tolerate high-intensity therapy. The moderate intensity option for those over 75 years of age was included as these individuals are prone to more adverse side effects and are often on several medications that could lead to adverse drug-drug interactions.¹
Those individuals over 21 years of age with an LDL-C of greater than 190mg/dL were recommended to be treated with high-intensity therapy. These recommendations were based on the rationale that these individuals may have a genetic hyperlipidemia, and their lifetime risk of ASCVD is high. The expert panel recognized that this particular subgroup had not been included in many of the randomized control trials but included the recommendation based on several studies indicating that for every drop of 39mg/dL of LDL-C, the risk of ASCVD decreased by twenty percent. With this in mind, the panel stated it would be reasonable to use high-intensity statin treatment to reduce the LDL-C by at least fifty percent.¹
The lifetime risk of ASCVD in diabetic individuals is much greater than the general population. Several studies have shown ASCVD risk reduction in diabetic patients who were placed on moderate-intensity statin therapy. However, trials involving high-intensity therapy did not include diabetic populations, and as a result the expert panel could not recommend high-intensity therapy based solely on the presence of diabetes. Accordingly, the panel used the 10-year ASCVD risk to further risk stratify which diabetic patients would benefit from high-intensity statin therapy. Those with a greater than 7.5% 10-year ASCVD risk were recommended for high-intensity therapy.¹
For those non-diabetic individuals between the ages of 40 and 75 years of age with LDL-C between 70 and 189mg/dL without clinical ASCVD, the expert panel noted the potential benefit of statin therapy in this group based on risk. The age limits were set based on the limited number of trials including subjects younger than 40 and older than 75 years of age. To further risk stratify individuals, the panel analyzed characteristics of the placebo groups in three large ASCVD primary prevention randomized control trials, which consisted of over 16,000 subjects.2,3,4 Using this data, the Pooled Cohort Equation was used to calculate an individual’s 10-year risk of ASCVD. Further meta-analysis was performed on statin randomized control trials. When analyzed with the 10-year ASCVD risk equation, those with a greater than 7.5% 10-year ASCVD risk showed a large risk reduction with treatment on moderate to high-intensity therapy.1
The intensity of statin therapy was determined after a meta-analysis was performed on randomized control trials evaluating ASCVD prevention that included various treatment regimens. The panel further classified statin therapies as high-intensity, moderate-intensity, or low-intensity based on estimated LDL-C reduction. High-intensity therapy estimated a fifty percent or greater reduction, moderate-intensity estimated a thirty to fifty percent reduction, and low-intensity estimated having a less than thirty percent reduction. The individual statins in their respective categories are as follows:
1. High-Intensity
a. Atorvastatin 40mg-80mg
b. Rosuvastatin 20mg-40mg
2. Moderate-Intensity
a. Atorvastatin 10mg-20mg
b. Rosuvastatin 5mg-10mg
c. Simvastatin 20mg-40mg
d. Pravastatin 40mg-80mg
e. Lovastatin 40mg
f. Fluvastatin XL 80mg
g. Fluvastatin 40mg twice daily
h. Pitavastatin 2mg-4mg
3. Low intensity
a. Simvastatin 10mg
b. Pravastatin 10mg-20mg
c. Lovastatin 20mg
d. Fluvastatin 20mg-40mg
e. Pitavastatin 1mg
The expert panel did identify several limitations within the dosing guidelines. Rosuvastatin 40mg, atorvavastatin 20mg, rosuvastatin 5mg, and pravastatin 80mg dosages were not analyzed in randomized control trials, but the dosages had been approved by the FDA. Atorvastatin was analyzed in only one trial at a 40mg dosage, and this was dose was only used if side effects were associated with an 80mg dosage.5
Following the ACC/AHA 2013 guideline release, the United States Preventive Services Task Force (USPSTF) released its own set of guidelines regarding the use of statins in 2016. The USPSTF focused on individuals that were without known cardiovascular disease and recommended low to moderate statin dosages for individuals age 40 to 75 years who had one of the following:
1. One or more cardiovascular risk factor (i.e., dyslipidemia, diabetes, hypertension, or smoking)
2. Calculated 10-year risk of a cardiovascular event greater than 10% (as determined by the Pooled Cohort Equation)
The USPSTF guidelines considered a 10-year risk of cardiovascular event greater than 10% a class B recommendation for statin therapy as there was sufficient evidence suggesting benefit for this group. However, there was less compelling evidence regarding individuals with a 10-year risk between 7.5% and 10%, and statin therapy for this group was subsequently given a class C recommendation, which differed from the recommendations of the ACC/AHA guidelines.
The USPSTF guidelines considered a 10-year risk of cardiovascular event greater than 10% a class B recommendation for statin therapy as there was sufficient evidence suggesting benefit for this group. However, there was less compelling evidence regarding individuals with a 10-year risk between 7.5% and 10%, and statin therapy for this group was subsequently given a class C recommendation, which differed from the recommendations of the ACC/AHA guidelines.
Table 1 - Statin for Primary Prevention Guideline Recommendations:
ACC/AHA 2013 vs. USPSTF 2016
REVIEW OF LITERATURE
With the discrepancies between different guidelines, studies have been conducted to analyze the potential impact when applied to the population of the United States. One study in particular took data from National Health and Nutrition Examination Survey
(NHANES) dataset from 2009-2014 and applied each set of guideline recommendations to this population. Based on this dataset, full implementation of the USPSTF guidelines would result in an incremental increase of 15.8% of the U.S. population receiving statin treatment. This is in contrast to the ACC/AHA guidelines, which would lead to an incremental increase of 24.3% of statin users. This equates to a potential increase of 17.1 million individuals based on USPSTF recommendations versus 26.4 million individuals based on ACC/AHA recommendations, a difference of 9.3 million people.10
Despite the new guidelines from both sets of agencies promoting an increase in statin usage, adaptation of the new recommendations has occurred with mixed results. Several studies have analyzed the impact of ACC/AHA recommendations since their release nearly four years ago. Using pharmacy and medical claims, a large health insurance organization found that half of high-risk individuals were not treated with a statin and eighty percent of individuals 75 years or younger with ASCVD were not receiving high-intensity statin therapy.11 In another study involving veteran patients with ASCVD, there was only a thirty-five percent increase in high-intensity statin use after discharge and even lower rates among Hispanics, Native Americans, elderly, and women.12 Furthermore, an analysis of Medicare beneficiaries who were hospitalized for acute coronary syndrome found that only twenty-seven percent were discharged from the hospital with a prescription for a high intensity statin, and another study demonstrated that even fewer beneficiaries were on high intensity statin therapy 2 years after a myocardial infarction.13,14 One study evaluated over 90,000 individuals with ASCVD diagnoses and found that statin usage actually decreased from thirty-two to thirty-one percent after the release of the guidelines and that high-intensity statin usage increased by only four percent.15
Reasons for the lower than expected adoption of the guidelines are not completely understood, although slow adoption of guidelines is not a new trend.16 One study suggested that there is a gap in physician understanding of the guidelines, with fifty-two percent of providers having not read the guidelines or a summary of the guidelines despite their widely publicized release.17 Another possibility is that healthcare providers are not familiar with the classification of statin intensity. A study published in 2016 found that seventy-one percent of practicing providers surveyed did not understand the definitions of low, moderate, or high intensity statin therapy.18 Finally, perhaps it is simply too soon to expect full implementation as the Institute of Medicine states it can take up to seventeen years for guidelines to be fully accepted into practice.19
CONCLUSION
According to the Centers for Disease Control (CDC) and World Health Organization, atherosclerotic cardiovascular disease remains the leading cause of death in the United States and worldwide.20,21 It has been estimated that over 15.5 million individuals in the United States alone have coronary artery disease. Every forty-two seconds an American will have a myocardial infarction, and of these, one-third will die as a result.22 It has been well documented that statin therapy reduces major adverse cardiovascular events in those with or at risk of ASCVD. A meta-analysis evaluating statin effectiveness in twenty-seven randomized trials involving 174,000 participants showed a reduction in all-cause mortality. This was primarily driven by reductions in deaths due to coronary artery disease, with a twenty percent relative risk reduction, and other cardiac causes, with a ten percent relative reduction.23
With the burden of ASCVD present, physicians should continue to prioritize prevention and treatment using lifestyle modification, risk factor reduction, and if warranted, appropriate statin therapy.
REFERENCES
1. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol
to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart
Association Task Force on Practice Guidelines. Circulation. 2014;129
2. Downs J, Clearfield M, Weis S et al. Primary prevention of acute coronary events with lovastatin
in men and women with average cholesterol levels. Results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998; 279:1615-1622.
3. Nakamura H, Arakawa K, Itakura H et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective
randomised controlled trial. Lancet 2006; 368:1155-1163.
4. Ridker PM, Danielson E, Fonseca FAH et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195-207.
5. Pedersen TR, Faergeman O, Kastelein JJP et al. High-dose atorvastatin vs usual-dose simvastatin for secondary
prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005; 294:2437-45.
6. Rana JS, Tabada GH, Solomon MD, et al. Accuracy of the atherosclerotic cardiovascular risk equation in a large
contemporary, multiethnic population. J Am Coll Cardiol. 2016;67(18):2118-2130.
7. Cook NR, Ridker PM. Further insight into the cardiovascular risk calculator
controversy: the roles of statins, revascularizations, and under-ascertainment in the Women's Health Study. JAMA Intern Med. 2014;174(12):1964-1971.
8. DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination
among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162(4):266-275.
9. Bibbins-Domingo K, Grossman DC, Curry SJ, et al; US Preventive Services Task Force. Statin use for the primary
prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316(19)1997-2007.
10. Pagidipati NJ, Navar A, Mulder H, Sniderman AD, Peterson ED, Pencina MJ.
Comparison of recommended eligibility for primary prevention statin therapy based on the US Preventive Services Task Force recommendations vs the ACC/AHA guidelines. JAMA. doi:10.1001/jama.2017.3416
11. Tran JN, Kao TC, Caglar T, et al. Impact of the 2013 cholesterol guideline on patterns of lipid-lowering treatment in patients with atherosclerotic cardiovascular disease or diabetes after 1 year. J Manag Care Spec Pharm. 2016;22(8):
12. Rodriguez F, Lin S, Maron DJ, Knowles JW, Virani SS, Heidenreich PA. Use of high-intensity statins for patients with ASCVD in the VA Health System. Am Heart J. 2016; 182:97-102.
13. Rosenson RS, Kent ST, Brown TM, et al. Underutilization of high-intensity statin therapy after hospitalization for coronary heart disease. J Am Coll Cardiol. 2015;65(3):270-277.
14. Colantonio LD, Huang L, Monda KL, Bittner V, Serban M-C, Taylor B, Brown TM, Glasser SP, Muntner P, Rosenson RS. Adherence to High-Intensity Statins Following A Myocardial Infarction Hospitalization Among Medicare Beneficiaries JAMA Cardiology April 19, 2017.
15. Okerson T, Patel J, DiMario S, Burton T, Seare J, Harrison DJ. Effect of 2013 ACC/AHA Blood Cholesterol Guidelines on Statin Treatment Patterns and Low Density Lipoprotein Cholesterol in Atherosclerotic Cardiovascular Disease Patients. JAMA March 2017, Volume 6, Issue 3
16. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458-1465.
17. Virani SS, Pokharel Y, Steinberg L, Chan W, Akeroyd JM, Gowani SA, Kalra A, Polsani V, Miedema MD,Jones PH, Nambi V, Petersen LA, Ballantyne CM. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol. 2016; 10:497-504.e494.
18. Bellows BK, Olsen CJ, Voelker J, Wander C. Antihyperlipidemic medication treatment patterns and statin adherence among patients with ASCVD in a managed care plan after release of the 2013 ACC/AHA guideline on the treatment of blood cholesterol. J Manag Care Spec Pharm.2016;22:892-900
19. Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
20. Kochanek KD, Murphy SL, Xu J, Tejada-Vera B, Division of Vital Statistics National Vital Statistics Reports, Vol. 65 No. 4, June 30, 2016
21. World Health Organization, Fact Sheet: Top 10 Causes of Death. January 2017.
22. Writing Group M, Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133:e38-360.
23. Cholesterol Treatment Trialists C, Mihaylova B, Emberson J, et al. The effects of lowering
LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomized trials. Lancet 2012;380:581-90.