Adverse Childhood Experiences (ACEs) Screening During Well-Child Checkups: Insights from a Student-Led Quality Improvement Project in the Rural Medical Track
Oula M Eldow, OMS-IV, Oklahoma State University for Health Sciences, College of Osteopathic Medicine - Tulsa, Rural Medical Track
Krista Schumacher, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Corresponding Author:
Oula M Eldow, OMS-IV
281-256-5978
oeldow@okstate.edu
OSU College of Osteopathic Medicine at Tulsa
Disclosures: This work was partially funded by the Health Resources and Services Administration’s Medical Student Education Training Program (Grant T99HP52102). There are no conflicts of interest to disclose.
Abstract
Background
Early identification of adverse childhood experiences (ACEs) is critical to long-term health, yet ACEs screening is rarely integrated into routine well-child checkups (WCCs). This quality improvement (QI) project explored the feasibility of implementing the Pediatric ACEs and Related Life-events Screener (PEARLS) during WCCs and assessed its educational value for a third-year medical student.
Methods
PEARLS forms were distributed during WCCs over a four-week rural clinical rotation. Implementation was guided by the Plan-Do-Study-Act cycle, with the student leading each phase.
Results
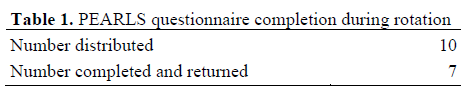
Of 10 screeners distributed, 7 were completed and saved to patients’ records. The process did not disrupt the clinic’s workflow or interfere with the student’s responsibilities.
Conclusions
This project provided hands-on QI experience for the student and suggests that ACEs screening may be integrated into primary care with minimal disruption. Brief QI projects during clinical rotations can deepen students’ understanding of practice improvement and encourage meaningful contributions to clinical care.
Keywords: undergraduate medical education, quality improvement, PEARLS, ACEs, preventative screening
Introduction
Quality improvement (QI) projects are increasingly being incorporated into undergraduate medical education to train future physicians in assessing and improving patient care.1 Short-term, student-led QI efforts provide valuable hands-on experience, especially in underserved or rural settings where flexible, low-cost adjustments can have immediate effects.2 Such projects often include adding health screenings to clinic visits or increasing patients screened with existing assessments.3,4 This paper describes a student-led QI project that introduced screening for adverse childhood experiences (ACEs) into pediatric visits during a clinical rotation.
The Pediatric ACEs and Related Life-events Screener (PEARLS) is an evidence-based tool developed to facilitate identification of ACEs in pediatric populations.5 ACEs such as family substance abuse or exposure to domestic violence are significant contributors to poor health outcomes well into adulthood.6 In 2023, more than one in five Oklahoma children experienced ACEs, the second-highest rate in the nation.7 Despite recommendations from the American Academy of Pediatrics,8 ACEs screening in clinical settings remains underused. Barriers range from time constraints to concerns about the sensitivity of the subject matter.9
This study, developed during the OSU College of Osteopathic Medicine (OSU-COM) elective course CLME 8132 Early Research Experience (ERE), evaluated whether integrating PEARLS into well-child checkups (WCCs) was feasible and if it could provide a meaningful educational experience in QI planning and execution for the student investigator and first author (OE).
Using the Institute for Healthcare Improvement’s Plan-Do-Study-Act (PDSA) model,10 the ERE course integrates QI instruction into the curriculum for students in the rural, tribal, and urban underserved medical tracks at OSU-COM. Students who complete the course are eligible for a research rotation with the course instructor and second author (KS) that involves implementing QI projects during clinical rotations. This approach aligns with the need to engage students in the practice of QI to understand potential obstacles of integrating change into clinical workflows.11
Methods
The project was implemented at Great Salt Plains Health Center, a rural Federally Qualified Health Center in Enid, Oklahoma, in the spring of 2024 during a required four-week rotation for Rural Medical Track students. Per OSU-CHS Institutional Review Board guidance, QI projects solely intended to improve health outcomes do not qualify as human subjects research;12 therefore, this project was not submitted for IRB approval.
In the PDSA cycle’s planning phase, the student and preceptor collaborated to integrate PEARLS into the clinic’s routine workflow. PEARLS questionnaires were distributed on days when the medical student was present. After families had been roomed, either the nurse or the preceptor and student gave guardians the PEARLS along with other visit paperwork. Before the visit began, either the nurse or medical student explained its purpose, with the preceptor providing additional information as needed.
During implementation (the “do” phase of the PDSA), the student refined the process based on daily observations, such as adjusting who introduced the screener and how it was described to families. Guardians were asked to complete the questionnaire during the visit and return it with other visit paperwork. As part of the PDSA “study” phase, the student tallied completed questionnaires and filed them in patients’ medical records. For the PDSA “act” phase, no formal changes to the clinic’s workflow were made given the short project duration.
Results
As shown in Table 1, of the 10 PEARLS questionnaires distributed, 7 were completed and returned.
As a follow-up to project completion, the student and preceptor discussed how well the screener’s integration meshed with existing workflows. Because the PEARLS discussion took only a couple of minutes and was part of routine paperwork, implementation did not affect visit flow. The process did not require extra staff or interfere with the student’s other responsibilities. In addition, providers reported that completed PEARLS questionnaires provided useful information for patient care. The student and preceptor also discussed minor improvements, such as introducing PEARLS earlier in the intake process, to improve uptake and integration should the clinic adopt the screening long-term.
Discussion
The results suggest that offering PEARLS alongside standard visit paperwork could be an effective strategy for collecting information on ACEs in the pediatric setting. This aligns with existing research that shows families are generally willing to participate in ACEs screening when presented with a user-friendly tool in a supportive clinical environment.9,13
This project had a few limitations. With four weeks to conduct the project, and forms being distributed only when the medical student was present, the sample size was too small to draw firm conclusions about the feasibility of integrating PEARLS into WCCs. Further, of the 10 PEARLS questionnaires distributed, 3 were not completed. This could reflect confusion with the clinic’s existing paperwork, which includes a standard screener, making the PEARLS seem duplicative. Another possibility is that some guardians may have been hesitant to disclose sensitive experiences due to concerns about stigma, shame, or judgment by clinic staff—all barriers identified in prior ACEs screening studies.13
The project gave the student direct experience applying the PDSA model in a clinical setting. Didactic QI training and applied experience leading a project provided the student with the tools and understanding necessary for engaging in QI activities required during residency.14
Conclusion
The project highlighted the feasibility and educational value of conducting short-term QI projects during clinical rotations. By leading this project, the medical student gained practical experience in QI planning and implementation, collecting and recording data, and engaging in scholarly activities.
The findings from this project suggest that ACEs screening during WCCs may be feasible and help identify risks some pediatric patients may face. The student gained a deeper understanding of how to identify and test small but meaningful changes and laid the groundwork for a potential longer-term QI project during residency.
The ERE course, combined with leading QI projects, reinforces students’ awareness of opportunities to improve health care for marginalized and underserved populations. Exposure to QI initiatives during medical education enhances students’ understanding of QI principles and prepares them for residency and future practice. This experience underscores the importance of embedding hands-on QI opportunities into medical curricula to build future physician capacity for improving patient care.
Acknowledgements
Thank you to Nicholas Hoffsommer, DO, adjunct faculty in family medicine for the OSU-COM, for his support of this project.
REFERENCES
1. Herman DD, Weiss CH, Thomson CC. Educational strategies for training in quality improvement and implementation medicine. ATS Sch. 2020;1(1):20-32. doi:10.34197/ats-scholar.2019-0012PS
2. Stubbs C, Ward B. The role of medical student quality improvement projects in health care: A scoping review. Aust J Rural Health. 2025;33(1):e70009. doi:10.1111/ajr.70009
3. Butala NM, Chang H, Horwitz LI, Bartlett M, Ellis P. Improving quality of preventive care at a student-run free clinic. PLoS One. 2013;8(11):e81441. doi:10.1371/journal.pone.0081441
4. Dolfini L, Williamson G, Oakeshott P. Including medical students in quality improvement projects in primary care. Future Healthc J. 2020;7(2):155-156. doi:10.7861/fhj.2019-0049
5. Koita K, Long D, Hessler D, et al. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: A pilot study. PLOS ONE. 2018;13(12):e0208088. doi:10.1371/journal.pone.0208088
6. Centers for Disease Control and Prevention. About Adverse Childhood Experiences. Adverse Childhood Experiences (ACEs). January 31, 2025. Accessed February 20, 2025. https://www.cdc.gov/aces/about/index.html
7. U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). United Health Foundation. America’s Health Rankings analysis of National Survey of Children’s Health 2022-2023. Accessed February 14, 2025. https://www.americashealthrankings.org/explore/measures/ACEs_8_overall/OK
8. Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232-246. doi:10.1542/peds.2011-2663
9. Bright MA, Alford SM, Hinojosa MS, Knapp C, Fernandez-Baca DE. Adverse childhood experiences and dental health in children and adolescents. Community Dent Oral Epidemiol. 2015;43(3):193-199. doi:10.1111/cdoe.12137
10. Ogrinc GS, Headrick LA, Barton AJ, Dolansky MA, Madigosky WS, Miltner RS. Fundamentals of Health Care Improvement: A Guide to Improving Your Patients’ Care. 3rd ed. Joint Commission Resources, Institute for Healthcare Improvement; 2018.
11. Carter J, Capon S, Dyer C, Whittaker M. Quality improvement in the undergraduate medical curriculum: The need for clinical exposure. BMC Med Educ. 2021;21(1):467. doi:10.1186/s12909-021-02566-2
12. Oklahoma State University Center for Health Sciences. HRP-820 investigator guidance: Quality improvement activities in health care. Human Subjects Research, Investigator Guidance. January 28, 2019. Accessed September 9, 2024. https://medicine.okstate.edu/research/human-subjects-research/hrp/hrp-820-investigatorguidance-quality-improvement-activities.pdf
13. Kapke TL, Karst J, LiaBraaten B, et al. Family caregiver acceptability of assessing caregiver Adverse Childhood Experiences (ACEs) and distress in pediatric specialty care. Children (Basel). 2023;10(2):382. doi:10.3390/children10020382
14. Bodenheimer T, Dickinson WP, Kong M. Quality improvement models in residency programs. J Grad Med Educ. 2019;11(1):15-17. doi:10.4300/JGME-D-18-00556.1