Superior Vena Cava Syndrome in The Setting of A Cavitary Lesion with Mediastinal Invasion: A Case Report
Bryan Wright, DO,Diagnostic Radiology
Josh Moore, DO,Diagnostic Radiology
Jonathon Kirkland, DO, Diagnostic Radiology
Corresponding Author: Bryan Wright, DO, PGY-3 Radiology Resident; bdwrigh@okstate.edu, 744 w 9th St, Tulsa, Oklahoma, 74127
Institutions: Oklahoma State Medical Center
Funding: None
Conflicts of Interest: There were no conflicts of interest associated with this case report.
Background: Partial or complete occlusion of the Superior Vena Cava (SVC) can lead to a sequela of symptoms and associated imaging findings known as SVC syndrome. Common clinical findings of SVC syndrome include facial redness, upper extremity swelling, neck edema, facial edema, venous distension, dyspnea, headache, and blurred vision. The most common cause of SVC syndrome is malignancy with a recent uptick in cases related to medical devices such as pacemakers or defibrillator leads. 1 In the clinical setting suspicious for SVC syndrome, CT imaging is the imaging modality of choice with both sensitive and specific findings for SVC syndrome. 3
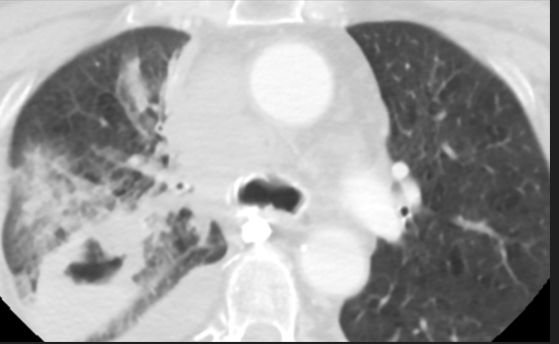
Case Presentation: A 71-year-old female initially was seen for a palpable lump of her right neck in the outpatient setting. This was discovered after the patient had been complaining about worsening headaches and neck pain in recent months. An ultrasound was performed which revealed a vascular mass of the right neck with the recommendation for CT imaging of the neck with contrast. CT imaging revealed a cavitary lesion within the right upper lung lobe with extension into the mediastinum. The mediastinal mass was only partially visualized. Both mass effect and likely invasion of the SVC were present. Extensive vascular collaterals within the right neck, axilla, and paravertebral space appeared to communicate with a prominent azygous vein. Questionable thrombosis of the right brachiocephalic vein was also present with assessment limited secondary to imaging technique.
A dedicated chest CT with contrast was recommended and the ordering physician was contacted with these results. The patient was immediately contacted and reported to the primary care office. At the time of physical exam the patient reported increasing shortness of breath when leaning forward. The patient would proceed to go into cardiac arrest at this time. Resuscitation efforts were successful. The patient was admitted to a different hospital where it was discovered on CT chest with contrast that the patient did in fact have SVC invasion with tumor thrombus in the right atrium. Mass effect was also present on the right pulmonary artery with additional extension into the right bronchus. Endobronchial biopsy was performed revealing Non-Small Cell Carcinoma. The patient would subsequently pass away a short time after this.
Discussion: The case presentation demonstrates the importance of CT examination in the diagnosis of SVC syndrome and common findings of SVC syndrome. The formation of vascular collaterals such as in our case is highly associated with symptomatic SVC syndrome. 1 CT examination, much like in our case, not only can reveal the causative pathology, but can also demonstrate the extent of disease burden. Furthermore, this case demonstrates the rapid progression of morbidity and mortality associated with SVC syndrome. While not performed at our imaging center, due to the patient not being present, ultrasound is critical to further exclude thrombosis of the subclavian, axillary, and jugular veins. 2
Conclusion: The presence of symptoms clinically suspicious for SVC syndrome should raise concern for malignancy. Furthermore, it is imperative that CT imaging to assess for disease burden and the level of obstruction is performed. Ultrasound imaging should also be used to rule out deep venous thrombosis of the subclavian, jugular, and axillary veins.
Keywords: superior vena cava syndrome, malignancy, radiology


Reference:
1.Azizi AH, Shafi I, Shah N, et al. Superior Vena Cava Syndrome. JACC: Cardiovascular Interventions. 2020;13(24):2896-2910. doi:https://doi.org/10.1016/j.jcin.2020.08.038
2. Shah RP, Bolaji O, Duhan S, et al. Superior Vena Cava Syndrome: An Umbrella Review. Cureus. 2023;15(7). doi:https://doi.org/10.7759/cureus.42227
3. Seligson MT, Surowiec SM. Superior Vena Cava Syndrome. PubMed. Published 2020. https://www.ncbi.nlm.nih.gov/books/NBK441981/
4. Shah RP, Bolaji O, Duhan S, et al. Superior Vena Cava Syndrome: An Umbrella Review. Cureus. 2023;15(7). doi:https://doi.org/10.7759/cureus.42227