Healing After Stillbirth: The Intersection of Faith, Race & Healthcare
Reem Babikir, EMBA

Corresponding Address: Reem Babikir, Oklahoma State University, Center for Health Sciences, Doctoral Program in Healthcare Administration, Tulsa, OK-74107, Reem.Babikir@OKstate.edu
Funding Sources: This research did not receive funding from any source.
Conflicts of Interest Disclosures: The author declares no conflict of interest relevant to this research.
Abstract:
Background-
Stillbirth is defined by the American Medical Association (AMA) as the death or loss of a baby at or beyond 20 weeks of the pregnancy gestation period.1 The identification of the gestational period is significant as it is the primary variable in classifying the pregnancy loss as a stillbirth rather than a miscarriage. This separation is vital because although both terms signal the death of a fetus, the gestational age variable contributes to a profoundly distressing experience for the parents and has different clinical implications. Although many recent studies address various factors such as maternal health, fetal complications, and healthcare practices that contribute to stillbirth incidence, there has not been enough research about the aftermath and recovery of stillbirth for mothers and families across different variables, such as racial and religious affiliations and socioeconomic levels. Remarkably, there is a significant research gap in understanding the psychosocial experiences of Muslim Women of Color (WOC) after stillbirth, which this study aims to address.
Methods-
A convergent mixed-method review methodology was utilized for this study, involving a comprehensive analysis of existing primary and secondary source literature from the years 2010 to 2024, consisting of research articles, scientific studies, and journal articles on the psychosocial experiences of Muslim women following pregnancy loss, their religious beliefs and practices, and the support provided by faith communities and spiritual leaders. Information gathered that is germane to the proposal included identifying religious denomination data, the role of community in the healing journey, exploring the lived experience of Muslim female patients in the West, a descriptive review of stillbirth management guidelines from the American College of Obstetricians & Gynecologists (ACOG), the Royal College of Obstetricians & Gynecologists (RCOG), exploring the impact of burnout, emotional health, and mental health on OBGYN physicians medical decisions and risks of malpractice lawsuits in correlation with low physician empathy scores and patient dissatisfaction. The data gathered resulted in a thematic analysis of existing literature supporting new recommendations for stillbirth management protocols in healthcare settings, designing clinical spaces that accommodate patients who experienced stillbirth, and providing holistically adequate stillbirth support for bereaved mothers and families.
Results-
Findings highlight gaps in the consistency of stillbirth management, the need for culturally competent care, and the importance of suitably designed clinic spaces for grief privacy. They also emphasize the influence of faith-based healing. Additionally, factors such as physician burnout and unconscious bias related to cultural context and appearance can significantly influence outcomes in cases of neonatal death and stillbirth, contributing to disparities in maternal-fetal healthcare.
Conclusion-
This review highlights the urgent need for healthcare systems, providers, and policymakers to develop comprehensive, culturally and religiously sensitive frameworks for stillbirth aftercare. It also underscores the need to create effective policies that address maternal disparities among Women of Color (WOC) and ensure that healthcare professionals (HCPs) receive adequate support for their well-being, which also influences neonatal and maternal outcomes.
Study Introduction:
Pregnancy loss, encompassing miscarriage, stillbirth, and other forms of fetal demise, represents a critical global public health issue, significantly impacting the emotional and psychological well-being of affected women and their families. Stillbirth, which is the loss of a baby at 20 weeks of pregnancy or beyond, is an especially devastating event.1 According to Adeleye (2024), the estimated prevalence of 13.9 stillbirths per 1000 total births translates to nearly 2 million stillbirths annually.2 The psychological consequences of such losses include heightened anxiety, stress, and depressive symptoms (Cuenca, 2023; Reardon & Craver, 2021; Mendes et al., 2023; Herbert et al., 2022).2 These emotional repercussions often extend beyond physical recovery (Farren et al., 2018),2 with additional complexities introduced by cultural, religious, and demographic factors (Nynas et al., 2015; Crockett et al., 2021).2
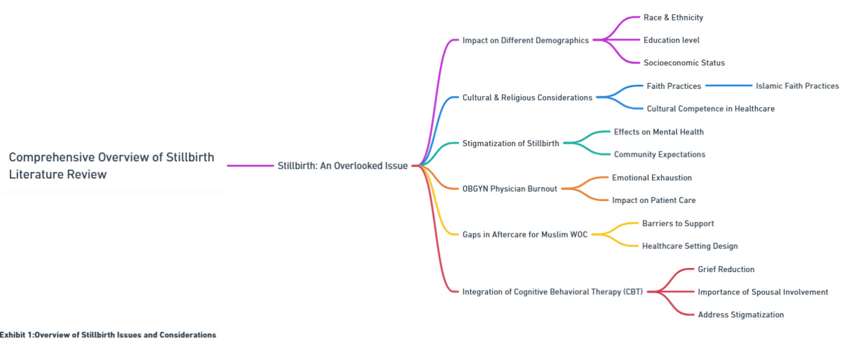
Religion and spirituality can provide significant comfort and guidance during periods of grief. Research indicates that religious beliefs and practices can facilitate coping during pregnancy loss.3 This literature review particularly highlights the potential positive impact of faith and community support in navigating pregnancy loss for Muslim women, offering structured frameworks that incorporate practices such as funeral rites and communal mourning (Exhibit 1).
Purpose of Study-
With the global Muslim population projected to reach 2.2 billion by 2030 (Von Grunebaum, 2016),2 it is increasingly important to understand the cultural and religious contexts that shape the experiences of pregnancy loss among Muslim women. Cultural and religious emphases on pronatalism and women's reproductive roles can lead to feelings of guilt and reduced self-esteem following a miscarriage, which is the loss of a baby before 20 weeks of gestation (Allahdadian & Irajpour, 2015; Sutan & Miskam, 2012; Omar et al., 2019).2
Therefore, the purpose of this study is to explore the multifaceted experiences of Muslim Women of Color (WOC) who have undergone stillbirth, focusing on the role of faith, religious and cultural sensitivity, and support systems. By employing a convergent mixed-method approach, the goal is to examine the impact of the Islamic faith and community support networks in facilitating healing. Additionally, the effect of religious and cultural insensitivity from healthcare providers and the unique challenges WOC face in healthcare settings are thoroughly examined.
The study also investigates the mental health effects of adverse experiences, the likelihood of seeking professional therapy, and the influence of education and socioeconomic status on the healing process. Moreover, using quantitative data, it explores the perceptions of care among Muslim women with complex medical histories, the role of unconscious bias, the correlation between physician burnout and stillbirth, and the relationships between race, education, and adverse pregnancy outcomes. The research assesses the prevalence of stillbirth support programs and evaluates how medical institutions can incorporate cultural and religious awareness into aftercare, considering institutional policies, legality, and malpractice insurance. Highlighted solutions include culturally and religiously sensitive healthcare practices, enhanced support programs, and targeted training for medical staff to improve the care and support for Muslim WOC experiencing stillbirth.
Significance of the Study-
The significance of the study is that it addresses critical gaps revolving around the overlooked maternal healthcare needs of underrepresented and marginalized populations. By understanding the unique issues of Muslim women of color (WOC) who experience stillbirth, we can extract insights about how the interconnectedness of faith, cultural insensitivity, unconscious bias, and inadequate healthcare support influence the healing journey and mental health outcomes for bereaved mothers and families.
Additionally, this literature review investigates the correlations between physician burnout, race, education, socioeconomic status, and adverse pregnancy outcomes, thereby highlighting systemic issues that contribute to disparities in healthcare. The findings can guide the creation of targeted training programs for medical staff to reduce bias and improve cultural competence. They also highlight the importance of patient and physician advocacy by setting up effective institutional policies and support programs that can improve healthcare delivery, enhance medical training and working conditions, and ensure comprehensive stillbirth aftercare tailored to the needs of diverse and underrepresented populations.
Discussion:
Importance of Cultural and Religious Context-
According to data from the World Religion Database in 2009, Muslims represented 5.7 percent of the U.S. and European populations.4 Therefore, to create more inclusive and equitable policy change that aids in understanding and remedying stillbirth aftermath, this population's cultural and religious background must be further studied and accounted for in creating and integrating new supportive frameworks.
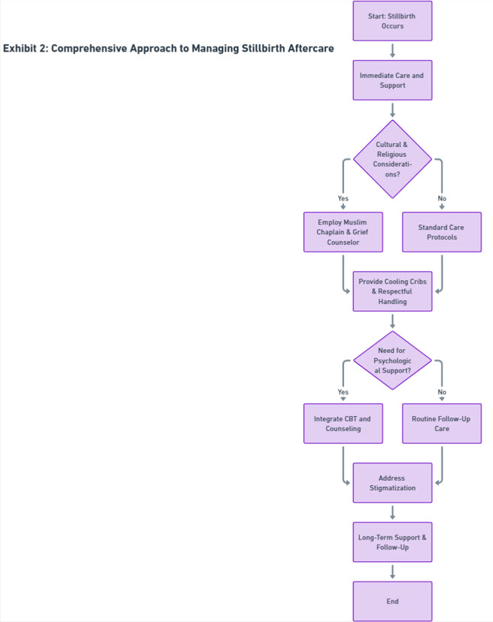
Understanding Stillbirth and Its Impact-
Furthermore, this literature review aims to provide a holistic view of the stillbirth experience and the recovery journey by addressing the correlation between the healthcare professionals' cultural misunderstanding and providing of inadequate support, the prevalence of OBGYN physicians' emotional exhaustion and burnout with the quality of care for women with complex medical histories; stillbirth and the delivery of compassionate care; the disparities between education levels and socioeconomic status in experiencing poorer outcomes; and finally, the correlation between cognitive behavioral-based counseling and the reduction in severity of grief symptoms in mothers and families after stillbirth. The following sections will address these views in more detail (Exhibit 2).
The Role of Healthcare Professionals-
Another crucial element for healthcare professionals (HCPs) to consider when dealing with bereaved mothers and families is that a central pillar of Islam is the surrender and acceptance of God’s will. This acceptance may be misinterpreted by HCPs as denial, given that acceptance is typically the final stage in the grief cycle. This misunderstanding can lead to conflicts in the care provided, exacerbating the agony of the stillbirth experience, and hindering necessary medical decisions. To address this, HCPs must demonstrate cultural competence by recognizing that acceptance is a religious duty, not a sign of denial. Empathetic communication protocols should be activated when managing such populations, and individualized care plans should be created to honor the family's religious beliefs while providing the necessary medical care and available options.
Importance of Cultural Competence-
Stigmatization of stillbirth is a critical variable that can be further studied to assess the degree of impact that it has when caring for Muslim WOC in particular. This stigma can exacerbate feelings of isolation, shame, and guilt among affected women, leading to adverse mental health outcomes and hindering their ability to seek necessary support and care. Moreover, cultural and religious sensitivities must be considered, as these women may face unique challenges related to their identities and community expectations. Understanding and addressing the stigmatization associated with stillbirth is essential for developing culturally competent healthcare strategies that provide comprehensive emotional and psychological support to Muslim WOC, thereby improving their overall well-being and recovery process.
Further research in this area can inform policies and interventions to reduce stigma and foster a more inclusive and supportive healthcare environment.
Impact on Quality of Care-
Caring for Muslim WOC who have experienced stillbirth can be particularly challenging for physicians, adding to their emotional exhaustion. These women may face unique cultural and religious challenges, requiring healthcare providers to be empathetic and culturally competent. The complex relationship between physicians' experiences of conflict and their emotional responses to work is not clearly understood. However, conflicts over treatment decisions, a manifestation of the lack of reciprocity in the physician-patient relationship, are thought to cause emotional stress that leads to exhaustion and burnout. Physicians with lower self-perceived empathy, females, and US-born physicians are likelier to report conflicts with patients.5 Those with lower self-perceived empathy report more conflicts, aligning with findings that a perceived lack of caring increases patient dissatisfaction and the risk of malpractice lawsuits.5
Strategies to Mitigate Burnout-
Addressing physician burnout is imperative to improving maternal and fetal health outcomes, particularly for marginalized communities. The American College of Obstetricians and Gynecologists (ACOG) has recognized the need for guidelines and interventions to support healthcare providers. ACOG recommends strategies such as promoting work-life balance, encouraging open discussions about mental health, and cultivating a supportive work environment by providing applicable support to mitigate the effects of burnout. Additionally, ACOG emphasizes the importance of implementing evidence-based practices and comprehensive care protocols to manage and prevent stillbirths effectively. By aligning these guidelines with efforts to reduce stigmatization and support both patients and healthcare providers, the healthcare system can enhance the overall quality of care and improve outcomes for all women, particularly marginalized communities.
Identifying Critical Gaps-
Despite the relatively low prevalence of stillbirth in high-income countries like the US, approximately 2 million babies are stillborn worldwide each year.6 This low stillbirth incidence rate in high-income regions may obscure the identification of critical gaps in the management and aftercare of stillbirth. For Muslim WOC in these countries, the challenges are even more pronounced due to cultural and religious stigmatization associated with stillbirth.7 These women often face unique barriers related to their identities and community expectations, which can exacerbate feelings of isolation, shame, and guilt.7 Therefore, global efforts to improve stillbirth aftercare must consider the broader context and include culturally competent strategies to effectively address these disparities and provide comprehensive emotional and psychological support to Muslim WOC.
Study Results:
Stillbirth as an Overlooked Issue-
Despite advancements in maternal-fetal medicine and related technological innovations, stillbirth remains an overlooked issue and is often undermined as a public health priority. Many studies have attempted to understand the cause and effect of stillbirth by assessing the impact of race, ethnicity, faith, disparities in income, education, and the soundness of the surrounding medical infrastructure. However, these efforts have yet to translate into significant policy changes or widespread awareness, highlighting the need for more comprehensive approaches to address and mitigate this critical issue.
Racial and Ethnic Disparities Related to Stillbirth-
The grieving experience and complex healing process following stillbirth transcend race, faith, and socio-economic status, affecting everyone from mothers to healthcare professionals in profound ways. However, the prevalence of stillbirth varies significantly across different regions and among women of color. Recent findings from a 2022 study, which examined over 2 million pregnancies from 20 high- and upper-middle-income countries, revealed stark disparities. The study found that Black women were twice as likely to experience stillbirth compared to White women, while Hispanic women faced a threefold increased risk of neonatal death.8 The same study also considered how a pregnant woman’s phenotype, skin color, and general cultural appearance contributed to discrimination at various levels in healthcare settings, such as unequal access to prenatal care, a disregard for patients’ health concerns by healthcare professionals, and delays in seeking care.8 Therefore, given that the Muslim faith encompasses people from diverse ethnicities and cultural backgrounds, healthcare professionals (HCPs) must have a fundamental understanding of how to approach this patient population and be aware of any underlying biases stemming from preconceived notions.
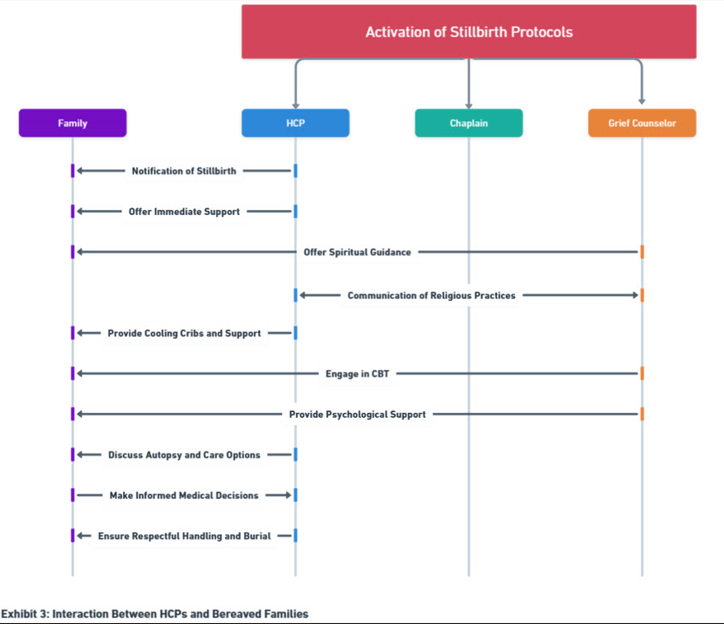
Cultural Misunderstandings in Healthcare-
A basic understanding of Islamic practices regarding death and burial, which are consistent across different ethnic and racial groups, equips healthcare professionals (HCPs) to manage interprofessional interactions effectively when a stillbirth occurs. For instance, hospitals and healthcare facilities can employ a Muslim chaplain as a spiritual counselor and the primary point of contact for communication between local Islamic centers and funeral homes.9 Recognizing that a deceased person's body must be treated with the utmost respect and dignity is essential to avoid unnecessary procedures or interventions. Therefore, hospitals should allocate resources and incorporate practices, such as providing cooling cribs, to preserve the baby's body while bereaved families spend limited time with it before burial proceedings commence. Additionally, HCPs should consider the psychological impact of avoiding unnecessary interventions on the body if a stillbirth autopsy option is presented and account for that in their care approach. Internal conflicts and additional psychological and emotional turmoil may arise for bereaved mothers and families torn between seeking scientific answers for their child's death following a stillbirth and honoring their child's body by limiting or eliminating physical medical interventions. This dilemma, which may scar the body and delay the burial, can leave parents with unanswered questions and a lack of closure about why the stillbirth occurred. Having an onsite or on-call grief counselor informed about Islamic faith beliefs and practices could help mitigate these conflicts and provide essential support (Exhibit 3).
OBGYN Physician Burnout-
In a recent 2022 study, 36% of US obstetricians and gynecologists reported high levels of emotional exhaustion from their work, indicating that more than a third of all practicing OBGYN physicians in the USA are at high risk for burnout.5 Emotional exhaustion, considered the chief component of burnout syndrome, can severely impact the quality of care provided to patients. High-stress levels, long working hours, and the emotional toll of dealing with complex and often tragic cases, such as stillbirth, contribute to burnout. High stress, in turn, can lead to decreased patient satisfaction, increased medical errors, and, ultimately, poorer pregnancy outcomes.
Post-Study Insights and Recommendations for Improving Healthcare Settings:
Creating Supportive Spaces for Grieving Families-
Existential issues, such as the search for meaning and coping with the profound sense of loss, are particularly acute for Muslim WOC. Their faith may play a crucial role in their healing process, offering a framework to make sense of the tragedy. However, this faith can also impose community expectations and pressures that contribute to stigmatization. The stigmatization of stillbirth can lead to adverse mental health outcomes and hinder the ability of Muslim WOC to seek and receive the necessary support. Addressing this stigma involves creating an inclusive and supportive healthcare environment that actively works to dismantle these barriers.
To accommodate these needs, healthcare settings and maternity wards must be thoughtfully designed. Spaces should be created to provide privacy and dignity for grieving families, allowing them the necessary time and space to process their loss. Maternity wards should include quiet rooms or designated areas where families can gather, reflect, and receive counseling without the distractions of a busy hospital environment (Exhibit 4).
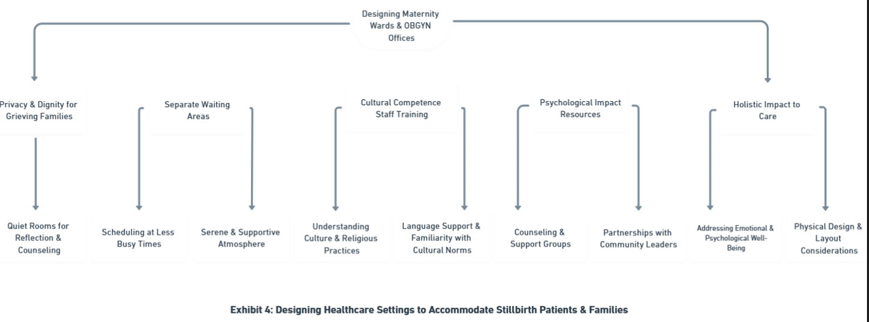
Cultural Competence Training-
Healthcare providers should design their office spaces for follow-up care to accommodate grieving mothers who may be experiencing PTSD from stillbirth and avoid triggers such as the sight of other pregnant women, newborn babies, and ultrasound technicians. Design elements can involve scheduling appointments at less busy times, separate waiting areas, and ensuring a serene and supportive atmosphere.
Cultural competence training for healthcare staff is crucial, ensuring they understand and respect the cultural and religious practices of Muslim WOC.10 Additionally, appointing staff members who speak the same language or are familiar with cultural norms can significantly enhance patients' comfort and trust.
Tailored Support and Counseling-
Healthcare providers should also be equipped with resources and protocols to address the psychological impact of stillbirth, offering counseling and support groups tailored to the specific needs of Muslim WOC. Partnerships with community leaders, non-profit and religious organizations can help bridge gaps in understanding and support, fostering a more holistic approach to care.
By incorporating these design elements and cultural considerations into healthcare settings, we can create a more supportive and inclusive environment that addresses not only the physical needs of Muslim WOC but also their emotional and psychological well-being. This holistic approach is essential for improving the overall quality of care and outcomes for all women, particularly those from marginalized communities.
Integration of Cognitive Behavioral Theory (CBT)-
Moreover, concerning psychological counseling, a study was conducted in 2017 aimed to assess the effectiveness of psychological counseling in reducing grief symptoms in mothers following a stillbirth, considering various factors such as education, socioeconomic status, and religious beliefs.11 Per the study, the intervention group that received psychological counseling showed a significant decrease in the severity of grief symptoms, including active grief, coping difficulty, and despair, compared to the control group that only received routine postnatal care.11 This aligns with prior research indicating the benefits of psychological support for grief alleviation. The study found that face-to-face interventions were more effective than non-face-to-face methods and highlighted the importance of spousal involvement and physical activity in reducing depression. The religious dimension of the intervention, which leveraged the participants' faith for coping, also contributed to its effectiveness. Negligence in hospitals and lack of peer support are identified as factors increasing vulnerability to mental illness post-stillbirth, emphasizing the need for comprehensive mental health services.11 Despite limitations such as a short counseling period, lack of long-term follow-up, and conducting the intervention during the early weeks of grief, the findings underscore the significant positive impact of cognitive behavioral therapy in reducing grief severity. Integrating psychological counseling, physical exercise, and religious support into postnatal care can help prevent complicated grief and better prepare mothers for future pregnancies.
Clinical Intervention Methods as Recommended By RCOG and SOGC-
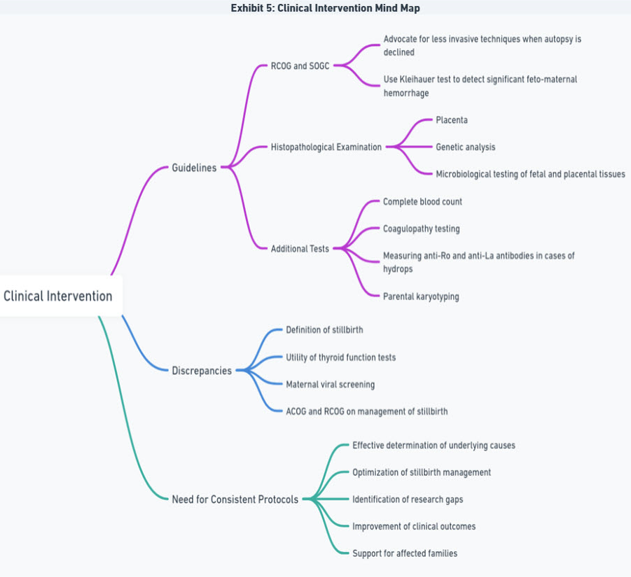
The Royal College of Obstetricians and Gynecologists (RCOG) and the Society of Obstetricians and Gynecologists of Canada (SOGC) advocate for less invasive techniques when autopsy is declined and suggest using a Kleihauer test to detect fetal red blood cells in the maternal circulation and verify if there was significant feto-maternal hemorrhage.12 Histopathological examination of the placenta, genetic analysis, and microbiological testing of fetal and placental tissues should be carried out. Additional tests such as complete blood count, coagulopathy testing (blood clotting test), and measuring anti-Ro and anti-La antibodies in cases of hydrops ( fluid buildup in a baby’s tissues and organs, causing swelling or edema), and parental karyotyping ( chromosomal analysis of both parents) are also recommended.12
However, discrepancies exist among the guidelines regarding the definition of stillbirth and the utility of thyroid function tests and maternal viral screening. Currently, only the ACOG and RCOG address the management of stillbirth; therefore, the development of consistent international practice protocols is crucial for effectively determining the underlying causes and optimizing the management of stillbirths. Identifying gaps in the current literature can highlight areas needing further research, thereby improving clinical outcomes and support for affected families (Exhibit 5).
Study Conclusion:
In conclusion, addressing the persistent issue of stillbirth requires a multifaceted approach that integrates policy changes, promotes inclusion of marginalized and underrepresented communities, and fosters advocacy opportunities to bridge the gap between HCPs and patients. It is imperative to create more inclusive and equitable policies that account for the cultural and religious backgrounds of diverse populations, particularly Muslim WOC. To this end, healthcare systems should implement comprehensive cultural competence training for HCPs, ensuring they understand and respect Islamic practices and the unique needs of Muslim patients. This training should include the hiring of Muslim chaplains and the provision of culturally sensitive support resources.
Policy changes should also focus on addressing the high prevalence of burnout among obstetricians and gynecologists, as this directly impacts the quality of care for patients experiencing stillbirth. Establishing guidelines and interventions that promote work-life balance, mental health support, and evidence-based practices will help mitigate burnout and improve patient outcomes. Additionally, there should be a concerted effort to reduce the stigmatization of stillbirth, particularly among marginalized communities, by creating supportive environments that offer comprehensive emotional and psychological support.
Advocacy opportunities focused on fostering partnerships between healthcare providers, community leaders, and religious organizations to enhance understanding and support for affected families should be created. Developing and implementing cognitive-behavioral therapy (CBT) programs tailored to the needs of grieving mothers and integrating these with physical and religious support can significantly reduce grief severity and prepare mothers for future pregnancies.
Overall, a holistic approach that combines policy reform, fosters inclusivity, and robust advocacy efforts is essential to bridge the existing gaps in stillbirth management and support. This will not only enhance the care provided to Muslim WOC and other marginalized groups but also contribute to a more compassionate and effective healthcare system for all.
Study Limitations:
Due to the nature of the population in question, the study faces significant challenges in obtaining relevant and reliable data. Complex medical histories, varying education levels, socioeconomic status, willingness to engage in cognitive-behavioral therapy (CBT), and high-context cultural characteristics contribute to the difficulty, compounded by the small sample size.
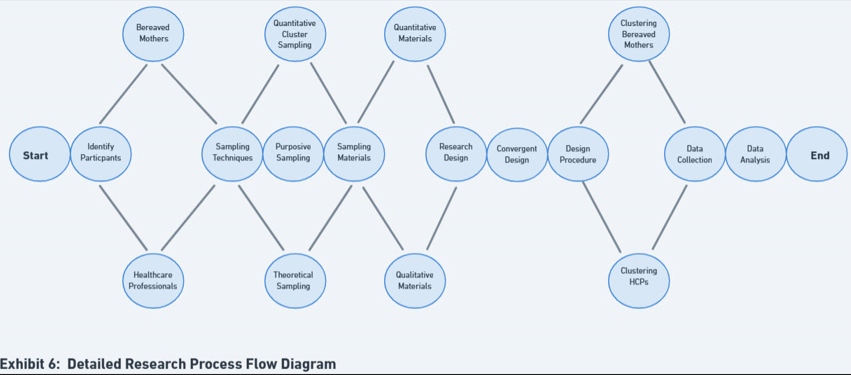
Despite these challenges, this research aims to provide a comprehensive understanding of the impact of stillbirth on both bereaved mothers and healthcare professionals. By employing a robust and ethically sound methodology, the study seeks to ensure the reliability and validity of its findings (Exhibit 6).
Additional Areas of Exploration:
Additional areas of exploration through further research include examining if bereaved mothers and families value respect in treatment over self-advocacy or would rather avoid conflict and how cultural context impacts these variables.
Proposal for Further Empirical Research Based on Study Results:
Methods-
This study utilizes a convergent mixed-methods review methodology, evaluating peer-reviewed studies published from 2010 to 2024. The research focuses on the psychosocial experiences of Muslim WOC following a stillbirth, examining cultural competence, faith-based support, and healthcare disparities. Moreover, this study lays down the framework for additional research based on the current findings.
Current and Future Participants-
With the potential to significantly contribute to the understanding of the experiences of Muslim Women of Color (WOC) who have experienced stillbirth and the healthcare professionals (HCPs) who have cared for them, this literature review aims to lay a foundation for employing an explanatory or exploratory sequential mixed methods approach for further areas of research. The current approach will delve into the psychological, social, and professional impacts of stillbirth, considering demographic, socioeconomic, and cultural factors, thereby inspiring the audience with the potential impact of this research.
Participants will involve bereaved mothers from diverse global geographies, including the USA, Canada, Europe, and Australia. Locally, participants will be categorized based on socioeconomic status (high and low), education level (ranging from high school diploma to graduate or professional degree(s)), race/ethnicity (African American, Asian, Caucasian, Hispanic non-white, Middle Eastern/North African, South Asian), age group (under 18, 18-30, 30-45, 45 and above), family type (nuclear, extended, tribal), and religious affiliation (active participants in spiritual practices such as daily prayers, fasting, and holiday celebrations, and non-active participants). Additionally, healthcare professionals participating in the study will include physicians (OBGYNS), nurses, hospital chaplains, psychologists/therapists/counselors, and funeral home professionals, focusing on their experience caring for stillbirth patients.
Participants Sampling Technique-
Using mixed methods sequential sampling approach for exploration, quantitative cluster sampling will be employed for both bereaved mothers and healthcare professionals. For bereaved mothers, the sampling will start with women with previous pregnancies, clustering based on adverse outcomes (stillbirth), race, age group, complex medical history, faith type, religious participation type, and family type. For healthcare professionals, the clustering will start with the kind of HCP (physician, nurse, administrator, therapist, chaplain) and experience with stillbirth patients. The qualitative component will use purposive sampling, selecting participants based on specific characteristics or qualities to gain an in-depth understanding of the research problem, and theoretical sampling, selecting participants based on emerging themes or theories during the research process.
Instruments-
Quantitative cluster sampling will involve comprehensive population lists, including census data, hospital records, and geographic databases, to provide demographic information and identify potential participants. Sampling frames for each cluster, geographic information systems (GIS) for mapping clusters, standardized surveys and questionnaires for data collection, and data management software like Excel, Statistical Package for Social Sciences (SPSS), or other database management systems will be employed to organize and analyze data. For purposive sampling, which allows for participant selection based on specific inclusion criteria that support an in-depth understanding of the research problem, detailed participant profiles, expert interviews, recruitment materials, screening tools, interview guides, informed consent forms, and reliable data recording devices will be used. Theoretical sampling that allows for participant selection based on emerging themes or theories during the research process will require access to initial data sources, coding software such as R ( a programming language and free software environment for statistical computing and graphics), Excel or ATLAS.ti for the management and analysis of qualitative data such as memos, focus group discussions, observations of behaviors and interactions in relevant settings, examination of policy papers, meeting minutes or personal diaries, and finally the incorporation of any existing literature reviews to identify gaps and potential areas of exploration. General considerations include obtaining ethical approval, training materials for researchers and data collectors, and precise and transparent data management plans to ensure data integrity and security.
Design-
Using the foundation of the convergent mixed methods design, additional collection of separate qualitative and quantitative data is required for comparison and identifying commonalities. The objective is to assess whether there is a difference in how religious versus non-religious mothers and families process the shock of stillbirth, whether HCPs were culturally informed about the target patient demographics, and if so, what effect that has on the standard of care and healing outcome. The quantitative component will measure the prevalence of stillbirth worldwide, compare it within different groups, and evaluate the degree of burnout among HCPs. The qualitative component will involve in-depth interviews to yield rich, profound data, offering a more transparent, more detailed picture of the subjects' experiences and helping to form connections that might explain the phenomena under investigation. The study's findings could lead to new healthcare practices and policies, thereby improving the standard of care for stillbirth and other similar conditions. The Exploratory and Explanatory Sequential Mixed Methods approach will be efficient, creating a platform for additional surveying and exploring new recommendation frameworks that emerge from the study. This approach facilitates a deeper understanding and paves the way for future research and practical applications.
Procedure-
The procedure will involve sequential clustering of bereaved mothers, starting with previous pregnancies, followed by adverse outcomes (stillbirth), race, age group, complex medical history, faith type, religious participation type, and finally, family type. Healthcare professionals will be clustered based on their role, their experience with stillbirth patients, and whether they are culturally informed. Sampling is influenced by specific characteristics or qualities required to gain an in-depth understanding of the research problem and emerging themes or theories that arise during the research process, commonly used in grounded theory studies.
Acknowledgments
I want to express my profound appreciation to Oklahoma State University's School of Health Sciences faculty. Their unwavering support and guidance during this term played a pivotal role in shaping my academic journey.
I am sincerely grateful to my husband, Mohammad Jangda; my mother, Thoraya Khidir; my sister, Rasha Babikir; my two sons; and my extended support system, Dina Ramadan and Cathryn McHenry. Your belief in my abilities and continuous encouragement has been instrumental in my healing journey and pursuit of a new career.
To my late father, Dr. Mohamed El Khawaga, your efforts and contributions to ensure dignified outcomes for your patients during your years of medical practice are not lost upon me.
I dedicated this research and journey in honor and cherished memory of my daughter, Kenzy Jangda. I hope that this work will benefit all mothers who have experienced or will experience stillbirths by serving as a valuable resource for healthcare professionals and assisting them in their care for these families.
References:
1. American Medical Association. Medical futility: Legal and ethical analysis. Virtual Mentor. 2007;9(5):375-383. https://doi.org/10.1001/virtualmentor.2007.9.5.msoc1-0705
2. Adeleye KK, Ogungbe O, Chutiyami M, Iradukunda F. Pregnancy loss among Muslim women: a narrative review. Int J Nurs Stud Adv. 2024;6:100205. doi:10.1016/j.ijnsa.2024.100205.
3. Murphy D, Flynn P, Warland J. Stillbirth and faith: when belief and death collide. J Pastoral Care Couns. 2021;75(1):33-39. https://doi.org/10.1177/1542305020962421
4. Grim BJ, Hsu B. Estimating the Global Muslim Population: Size and Distribution of the World's Muslim Population. Interdisciplinary Journal of Research on Religion. 2011;7. Available at: https://www.religjournal.com/pdf/ijrr07002.pdf
5. Yoon JD, Rasinski KA, Curlin FA. Conflict and emotional exhaustion in obstetrician-gynaecologists: a national survey. J Med Ethics. 2010;36(12):731–735. https://doi.org/10.1136/jme.2010.037762
6. Persson M, Hildingsson I, Hultcrantz M, Kärrman Fredriksson M, Peira N, Silverstein RA, Sveen J, Berterö C. Care and support when a baby is stillborn: A systematic review and an interpretive meta-synthesis of qualitative studies in high-income countries. PLoS One. 2023;18(8):e0289617https://doi.org/10.1371/journal.pone.0289617
7. Burden C, Bradley S, Storey C, et al. From grief, guilt, pain, and stigma to hope and pride - a systematic review and meta-analysis of mixed-method research of the psychosocial impact of stillbirth. BMC Pregnancy Childbirth. 2016;16:9. https://doi.org/10.1186/s12884-016-0800-8
8. Sheikh J, Allotey J, Kew T, et al. Effects of race and ethnicity on perinatal outcomes in high-income and upper-middle-income countries: an individual participant data meta-analysis of 2,198,655 pregnancies. Lancet. 2022;400(10368):2049–2062. https://doi.org/10.1016/S0140-6736(22)01191-6
9. Attum B, Hafiz S, Malik A, et al. Cultural Competence in the Care of Muslim Patients and Their Families. StatPearls [Internet]. Published July 3, 2023. Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK499933/
10. Hassan SM, Leavey C, Rooney JS, et al. A qualitative study of healthcare professionals’ experiences of providing maternity care for Muslim women in the UK. BMC Pregnancy Childbirth. 2020;20:400. https://doi.org/10.1186/s12884-020-03096-3
11. Navidian A, Saravani Z. Impact of Cognitive Behavioral-Based Counseling on Grief Symptoms Severity in Mothers After Stillbirth. Iran J Psychiatry Behav Sci. 2018;12(1):e9275. https://doi.org/10.5812/ijpbs.9275
12. Tsakiridis I, Giouleka S, Mamopoulos A, Athanasiadis A, Dagklis T. Investigation and management of stillbirth: a descriptive review of major guidelines. J Perinat Med. 2022;50(6):796-813. https://doi.org/10.1515/jpm-2021-0403
Additional References:
• Data Services, NYU. Introduction to ATLAS.ti. Google Slides. Available at: https://docs.google.com/presentation/d/1hK3foqHIhNP9sStOiX4M0_DEzVx0mdRzHbgBy2-wg9U/edit?pli=1#slide=id.g41bc532cf2_0_936
• Babikir, R. Overview of Stillbirth Issues and Considerations. Whimsical.com. Internal document.
• Babikir, R. Comprehensive Approach to Managing Stillbirth Aftercare. Whimsical.com. Internal document.
• Babikir, R. Interaction Between Healthcare Professionals and Bereaved FamiliesWhimsical.com. Internal document.
• Babikir, R. Clinical Intervention Mind Map. Whimsical.com. Internal document.
Babikir, R. Detailed research process flow diagram. Whimsical.com. Internal document.