HPV Risk Perceptions and Knowledge Among Oklahoma Undergraduates: Implications for Vaccination Efforts
Krista Schumacher, PhD, Oklahoma State University Center for Health Sciences, Center for Rural Health
Tracy Freudenthaler, PhD, MPH
Cynthia D. Lamon, EdD, MPH, MS, Oklahoma State University
Danielle Manship, DO, Oklahoma State University Center for Health Sciences, Obstetrics & Gynecology Medicine Residency Program
Corresponding author:
Krista Schumacher
918-284-7276
krista.schumacher@okstate.edu
OSU Center for Rural Health
Disclosures: This work received no external funding support. There are no conflicts of interest to disclose.
Abstract
Background
HPV vaccination rates among young adults remain low. This study, guided by the Health Belief Model, examined Oklahoma undergraduates’ perceptions of HPV risk, risk factors, and HPV knowledge.
Methods
Surveys were administered to students aged 18-24 at two universities. Chi-square analysis assessed the relationship between vaccination status and perceived risk, while t-tests compared HPV knowledge scores across vaccination and perceived risk groups. Thematic coding was used to analyze responses to an open-ended question about HPV risk factors.
Results
Vaccination status was significantly associated with perceived risk. Of vaccinated respondents, 79% reported “below average” risk versus 60% of unvaccinated respondents. Vaccinated respondents had significantly higher HPV knowledge scores, but no significant differences were found between risk groups. Overall, HPV knowledge was low (mean score=47%). The most-cited factor for vaccinated respondents was the HPV vaccine (27%); for unvaccinated respondents it was not being sexually active (31%).
Conclusions
Regardless of vaccination status, respondents generally perceived their risk as low, yet most did not identify the HPV vaccine as a protective factor. Young adults who are not sexually active may hold a false sense of safety from HPV. Health care providers should emphasize that vaccination before sexual activity offers the best protection against HPV.
Keywords: Human papillomavirus (HPV), HPV infection, risk factors, HPV vaccine, vaccine hesitancy, vaccine delay
Introduction
In 2022, only 57% of female college students and 41% of male students were up-to date on vaccination for human papillomavirus (HPV), well below the Healthy People 2030 benchmark of 80%.1 According to the Centers for Disease Control and Prevention (CDC), HPV vaccination could prevent more than 90% of HPV-related cancers.2,3 As the most common sexually transmitted infection (STI),4 HPV is of particular concern for young adults, especially college-age students, who are disproportionately affected due to increased sexual activity.5,6
Low vaccination rates among this population have been attributed to cost, limited access to health care, lack of recommendation by a health care provider, vaccine hesitancy, and scant knowledge about the vaccine and HPV.1,7 For instance, in validated assessments at several U.S. universities, mean HPV knowledge scores were only 36%-49% among students.8–10 Additionally, a study of California students revealed that many were unaware the HPV vaccine was recommended up to age 26 or that it was available at the student health center.11 At a midwestern university, less than half of college students correctly linked HPV to various HPV-associated cancers, excluding cervical cancer.12
Many college students believe their risk for HPV as low despite knowing little about HPV or the vaccine.13–15 For example, some underestimate their risk due to being in monogamous relationships or not being sexually active.16–18 Others believe only frequent sexual encounters with multiple partners increases risk19 or that condoms fully prevent HPV transmission.19,20
Consequently, these misconceptions may lead students to view vaccination as unnecessary.21
Despite HPV awareness campaigns targeting young adults,22,23 inaccurate perceptions of HPV risk persist among college students, particularly by those in monogamous relationships, asexual students, and students who believe practicing safe sex is enough to protect them from HPV. These misconceptions clearly indicate the need for targeted educational interventions that can help align risk perceptions with actual risk and better inform vaccination decisions.
The purpose of this study was to explore perceptions of HPV risk among Oklahoma undergraduate students and identify factors students believe increase the risk for contracting HPV. In particular, this study investigated how vaccination status influenced perceptions of HPV risk and risk factors and examined differences in HPV knowledge by vaccination status and risk perceptions. Understanding student beliefs about HPV risk and the connections among knowledge, vaccination, and perceived risk can inform targeted interventions to increase HPV vaccination coverage and improve current HPV education. We hypothesized that vaccination status is associated with perceptions of HPV risk and knowledge of HPV and used the Health Belief Model (HBM)24 as a framework for examining perceived risk.
Methods
We used a subset of data from self-administered surveys disseminated via email in fall 2020 and fall 2021 to a convenience sample of undergraduates aged 18-24 enrolled at two Oklahoma universities. One survey was originally conducted for a dissertation study examining HPV knowledge and vaccination influences.25 The surveys were approved by each school’s Institutional Review Board and administered using Qualtrics.
Data analyzed for this study included only respondents who answered the qualitative question, “What factors influence your chance of getting HPV?” Two quantitative items measured HPV vaccine status (fully vaccinated, partially vaccinated [series started], not at all vaccinated, unsure) and perceived personal risk compared to peers (below average, average, above average). This approach to measuring risk has been used in previous studies.26,27We used a chi-square test to investigate whether perceived risk differed based on vaccination status and, if so, an odds ratio examined the strength of the association. To meet the chi-square assumption for expected cell count, the variable of HPV vaccine status was collapsed into two levels (fully vaccinated/started series, unvaccinated/unsure) as was the variable for perceived risk (below average, average/above average).
The survey included a 23-item HPV knowledge scale adapted from the HPV Knowledge Survey, a psychometrically validated instrument developed by Waller et al.28 The scale assessed knowledge of HPV in the following domains: 1) health consequences; 2) HPV and cervical screening; 3) symptoms; 4) causes, risk factors and transmission; 5) prevention and treatment; 6) prevalence; and 7) testing and vaccination. Response options were “True,” “False,” and “I don’t know.” Participants received one point for each correct response; points were summed to create a total knowledge score (range of 0-23) and converted to a percentage score. We used independent samples t-tests to assess differences in scores between vaccine status and perceived risk groups.
Responses to the qualitative question were coded using a priori themes that broadly categorized responses as related to protective factors only, risk factors only, or both protective and risk factors; odd, erroneous, and responses indicating no risk or no knowledge of risk factors were also grouped together. The four authors coded responses independently and then met to review coding and reconcile discrepancies. The authors collaborated on further grouping risk and protective categories into relevant themes that emerged from the analysis, reconciling discrepancies as coding progressed. Codes were combined into numerical variables to quantify risk and protective factors. SPSS v28 and Microsoft Excel 365 were used to analyze data and create new quantitative variables from thematic coding of qualitative data. Frequencies were examined for respondents who reported below average risk to better understand conceptions of risk and/or protective factors among this population.
Results
The analytic sample consisted of 340 respondents. As shown in Table 1, respondents were primarily white (69.4%) and female (75%) with an average age of 20.9. Most grew up in suburban or urban areas (60%).

Perceived Risk for HPV Infection
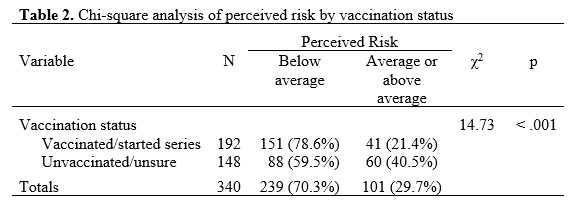
Table 2 shows the Pearson chi-square results and indicates that perceived risk was significantly different based on vaccination status (χ2 = 14.73, df = 1, N = 340, p < .001). Respondents who perceived themselves to be below average risk were more likely than expected under the null hypothesis to have been vaccinated or started the series than respondents who perceived themselves as average or above average risk. An odds ratio was computed (OR = 2.51, 95% CI[1.56, 4.04]) and indicated the odds of respondents perceiving themselves as below average risk if they had received or started the vaccine were 2.51 times the odds for those who were unvaccinated or unsure.
HPV Knowledge
Overall, scores on the HPV knowledge assessment (N=328) were low, with a mean score of 47%. For both independent samples t-tests, the homogeneity of variance assumption was met as assessed by Levene’s Test for Equality of Variances. The test for differences by vaccination status showed that scores for the vaccinated group (M=.51, SD=.22) were significantly higher (t=3.18, p=.002, d=.35) than scores for the unvaccinated/unsure group (M=.43, SD=.23). The test for differences by perceived risk showed that scores for the below-average group (M=.48, SD=.22) were not significantly different (t=1.20, p=.23, d=.15) from the average/above-average group (M=.45, SD=.24).
Qualitative Analysis: Factors Influencing Risk for HPV
Top-level coding frequencies for respondents who indicated their HPV risk as below average are presented in Table 3.
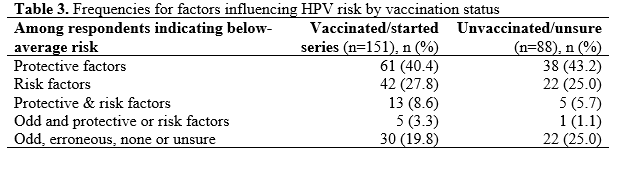
A slightly higher percentage of unvaccinated/unsure respondents cited protective factors while a somewhat larger percentage of vaccinated respondents cited risk factors or both protective and risk factors. The largest difference was for odd or erroneous factors or responses that indicated no risk factors or uncertainty of risk factors, with 25% of unvaccinated/unsure respondents reporting answers in this category compared to 19.8% of vaccinated respondents. Examples of these answers among unvaccinated/unsure respondents included, “I have not been sick before 6th grade,” “I eat healthy,” “Smoking,” “Everything,” “I have no idea,” and “I am not sure what HPV is.”
Among vaccinated respondents, examples included, “Long term use of oral contraceptive (birth control),” “Possibly genetics,” “The town that I lived in,” “I work in a higher risk environment delivering to people,” “…unsanitary needles such as when getting a tattoo or ears pierced,” “No clue,” “I am not sure as I have never been told,” and “I don’t do drugs?” In total, 22% of all respondents who perceived their risk to be below average, regardless of vaccination status, indicated they did not know HPV risk factors or did not feel they had any risk factors.
Subsequent coding categorized protective factors into themes of the HPV vaccine, safe sex, sexual abstinence, and monogamy; risk factors were grouped into themes of unsafe sex, multiple sexual partners, and any sex. Frequencies are shown in Table 4.
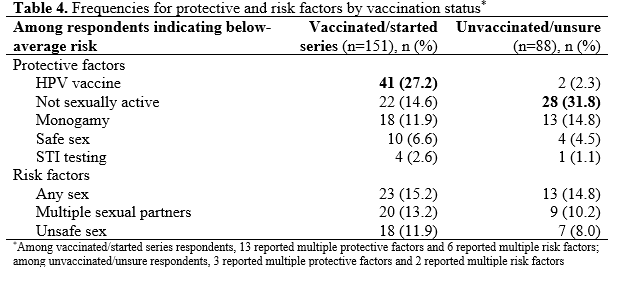
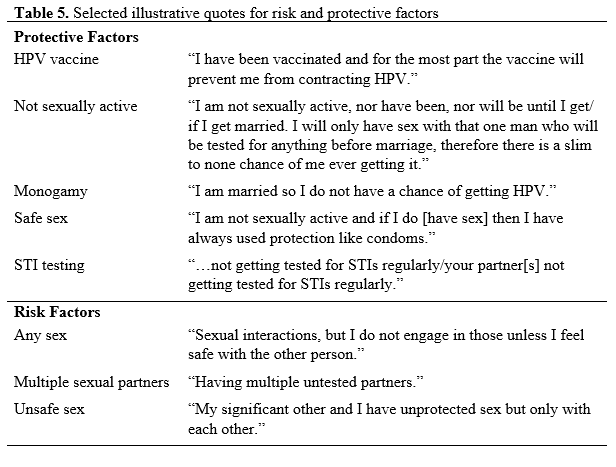
The most-reported protective factor among vaccinated respondents was the HPV vaccine (27%), while the top protective factor among unvaccinated/unsure respondents was sexual abstinence (32%). Only 2% of unvaccinated/unsure respondents noted the HPV vaccine as a protective factor, while about 15% of vaccinated respondents mentioned sexual abstinence as a protective factor. Monogamy was noted as a protective factor by a greater percentage of unvaccinated/unsure respondents at 15% versus 12% for vaccinated respondents, followed by safe sex at 7% of vaccinated versus 5% of unvaccinated/unsure. A very small percentage of both groups cited STI testing as a protective factor.
Differences were less pronounced for risk factors, with any sex the most-reported factor at about 15% for both groups, followed by multiple sexual partners and unsafe sex, with a greater percentage of vaccinated respondents mentioning these factors than unvaccinated/unsure respondents. Table 5 lists representative comments for protective and risk factors for both vaccination groups.
Discussion
This study investigated perceptions of HPV risk and related factors among Oklahoma undergraduate students, revealing a key finding: regardless of vaccination status, respondents generally perceived their personal risk of contracting HPV as low. Similar to other studies, ours found that vaccinated individuals had significantly greater HPV knowledge than unvaccinated individuals.29 However, HPV knowledge scores (mean=47%) were low regardless of vaccination status, suggesting that even vaccinated students may not fully understand the virus and how it is transmitted.30 In addition, knowledge scores did not differ by perceived risk group, suggesting that even students who believe they are at average or above average risk for HPV may not seek out information about the virus.10,13 These findings align with existing literature and present a significant challenge to increasing HPV vaccination rates on college campuses.
The qualitative findings shed additional light on these quantitative results. A notable percentage of all respondents—regardless of vaccination status—indicated they were abstinent or waiting until marriage to have sex. This suggests that students may judge their risk as low based on current behaviors without considering how future behaviors could affect their health.31 Several respondents believed condoms provide complete protection against HPV, demonstrating a lack of awareness of skin-to-skin transmission.32 A very small but noteworthy number of respondents indicated that STI testing reduced HPV risk, suggesting students may not understand that routine STI panels usually do not include HPV.33
The higher percentage of vaccinated respondents who cited the HPV vaccine as a protective factor versus the higher percentage of unvaccinated respondents reporting sexual abstinence as a protective factor underscores the importance of better vaccine education and promotion. Only a small percentage of unvaccinated respondents felt the HPV vaccine was a protective factor. Targeted efforts are needed to correct these misconceptions and highlight the importance of vaccination, regardless of current sexual activity.
From the lens of the Health Belief Model, our findings suggest that interventions should focus on increasing perceived susceptibility and perceived benefits of vaccination. Many students do not believe they are susceptible to HPV infection, and this belief is reinforced by inaccurate risk perceptions and limited knowledge of HPV transmission. Interventions that clearly communicate the potential consequences of HPV infection and the benefits of vaccination may be effective in increasing vaccine uptake.24
This study has implications for improving HPV prevention efforts among college students. Interventions should address not only knowledge gaps but also risk misperceptions and should communicate that vaccination is not just for those who plan to be sexually active.18 Health care providers, campus health centers, and student organizations should actively promote the HPV vaccine and provide accurate information about HPV risks and transmission.14 Tailoring educational materials and messages to address common misconceptions—such as the belief that monogamy or abstinence provide complete protection—may be particularly effective. Interventions should aim to increase not only knowledge but also the perception of personal susceptibility to HPV infection.
The results of this study should be interpreted in light of its limitations. Of the nearly 9,000 students who received the survey, only 478 responded. This may be due to several factors, including survey fatigue, survey length, and the sensitive nature of HPV as an STI. Because the study used a convenience sample of students from two Oklahoma universities, it may not represent all college students. Since the sample was predominately white and female, the results cannot be generalized to other populations. The study relied on self-reported data, which introduces the possibility of recall and social desirability biases. Because the study design was cross-sectional, no causal inferences can be made about the relationships between HPV risk perceptions, knowledge, and vaccination status.
From the standpoint of the survey design, the instrument did not ask for relationship status or level of sexual activity, although many provided this information on their own. Examining how respondents define “sexual activity” in connection to HPV risk may aid in understanding vaccine barriers and facilitators. In addition, the survey did not ask about religious background, which could help understand attitudes toward HPV risk and protective factors as related to religious or faith-based beliefs about sexual activity and pre-marital sex. Finally, the qualitative question—“What factors influence your chance of getting HPV?”—could have been more clearly worded to focus on HPV risk in general rather than factors specific to each respondent. This would have provided insight into students’ broader knowledge of HPV risk.
Conclusion
Health care providers play a critical role in tackling concerns and false information about vaccines. Several studies indicate that provider recommendations can significantly increase HPV vaccine uptake.34–36 Prior research using data from the same survey examined for this study found that reduced cancer risk was the most common reason for HPV vaccination given by providers.37 Because young adults may experience feelings of shame or stigma about vaccination since HPV is a sexually transmitted infection, adjusting vaccine guidance to highlight cancer prevention could enhance acceptance. Similarly, messaging that acknowledges whether someone is in a monogamous relationship or practicing abstinence could make young adults feel heard while also emphasizing that their current circumstances present the best opportunity for vaccination to be effective. By adopting these strategies, public health initiatives could increase acceptance of the HPV vaccine among college students.
References
1. Yoon S, Kim H, An J, Won Jin S. Exploring human papillomavirus vaccine hesitancy among college students and the potential of virtual reality technology to increase vaccine acceptance: A mixed-methods study. Front Public Health. 2024;12. doi:10.3389/fpubh.2024.1331379
2. Centers for Disease Control and Prevention. Cancers caused by HPV. HPV. September 30, 2024. Accessed February 16, 2025. https://www.cdc.gov/hpv/about/cancers-caused-by-hpv.html
3. Centers for Disease Control and Prevention. Cancers associated with human papillomavirus. U.S. Cancer Statistics. September 18, 2024. Accessed February 12, 2025. https://www.cdc.gov/united-states-cancer-statistics/publications/hpv-associated-cancers.html
4. Centers for Disease Control and Prevention. About genital HPV infection. Sexually Transmitted Infections (STIs). January 31, 2025. Accessed January 27, 2025. https://www.cdc.gov/sti/about/about-genital-hpv-infection.html
5. Office of Disease Prevention and Health Promotion. Sexually transmitted infections workgroup. Healthy People 2030. Accessed February 4, 2025. https://odphp.health.gov/healthypeople/about/workgroups/sexually-transmitted-infections-workgroup
6. Siegel DM, Klein DI, Roghmann KJ. Sexual behavior, contraception, and risk among college students. J Adolesc Health. 1999;25(5):336-343. doi:10.1016/s1054-139x(99)00054-3
7. McLendon L, Puckett J, Green C, et al. Factors associated with HPV vaccination initiation among United States college students. Hum Vaccin Immunother. 2021;17(4):1033-1043. doi:10.1080/21645515.2020.1847583
8. Nesser W, Ayodele O. Human papilloma virus knowledge among university students, staff, and faculty in the state of Indiana during 2016, 2019, and 2022. J Community Health. 2023;48(4):718-723. doi:10.1007/s10900-023-01210-y
9. Natipagon-Shah B, Lee E, Lee SY. Knowledge, beliefs, and practices among U.S. college students concerning papillomavirus vaccination. J Community Health. 2021;46(2):380-388. doi:10.1007/s10900-020-00922-9
10. Kasymova S, Harrison SE, Pascal C. Knowledge and awareness of human papillomavirus among college students in South Carolina. Infect Dis (Auckl). 2019;12:1178633718825077. doi:10.1177/1178633718825077
11. Kellogg C, Shu J, Arroyo A, et al. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Hum Vaccin Immunother. 2019;15(7-8):1760-1766. doi:10.1080/21645515.2019.1627819
12. Franca MC, Boyer VE, Gerend MA, et al. College students’ awareness of the link between human papillomavirus (HPV) and HPV-associated cancers. J Canc Educ. 2023;38(2):669-676. doi:10.1007/s13187-022-02172-w
13. Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. De Groot AS, ed. PLoS ONE. 2017;12(8):e0182266. doi:10.1371/journal.pone.0182266
14. Jin SW, Lee Y, Lee S, Jin H, Brandt HM. Factors associated with college students’ human papillomavirus (HPV) vaccination and preferred strategies for catch-up vaccine promotion: A mixed-methods study. Vaccines (Basel). 2023;11(6):1124. doi:10.3390/vaccines11061124
15. McMahon K. Using the Health Belief Model to Assess Undergraduate College Students Knowledge and Perceptions of Human Papillomavirus in Order to Better Understand Vaccine Intentions. Minnesota State University; 2018. https://cornerstone.lib.mnsu.edu/etds/769/
16. Thompson EL, Vamos CA, Straub DM, Sappenfield WM, Daley EM. “We’ve been together. We don’t have it. We’re fine.” How relationship status impacts human papillomavirus vaccine behavior among young adult women. Womens Health Issues. 2017;27(2):228-236. doi:10.1016/j.whi.2016.09.011
17. Waters AV, Merrell LK, Thompson EL. Monogamy as a barrier to human papillomavirus catch-up vaccination. J Womens Health. 2021;30(5). doi:10.1089/jwh.2020.8724
18. Adjei Boakye E, McKinney SL, Whittington KD, et al. Association between sexual activity and human papillomavirus (HPV) vaccine initiation and completion among college students. Vaccines (Basel). 2022;10(12):2079. doi:10.3390/vaccines10122079
19. Albright AE, Allen RS. HPV misconceptions among college students: The role of health literacy. J Community Health. 2018;43(6):1192-1200. doi:10.1007/s10900-018-0539-4
20. Hirschler C, Hope A, Myers JL. College students’ perceptions of and experiences with human papillomavirus and herpes: Implications for college sexual health education. American Journal of Sexuality Education. 2015;10(4):298-315. doi:10.1080/15546128.2015.1091760
21. Jensen JE, Wendt LH, Spring JC, Jackson JB. Human papillomavirus perceptions, vaccine uptake, and sexual risk factors in students attending a large public midwestern university. Vaccines (Basel). 2024;12(6):671. doi:10.3390/vaccines12060671
22. HPV Campus Vaccination Campaign. HPV Campus Vaccination Campaign. 2022. Accessed January 8, 2025. https://www.hpv-cvc.org/
23. HPV VAX NOW Young Adult Outreach Toolkit | Vaccines. Accessed January 15, 2025. https://www.vaccines.gov/get-involved/spread-the-word/toolkits/hpv-vaccine-promotional-toolkit/young-adults
24. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566-576. doi:10.1080/10410236.2013.873363
25. Freudenthaler T. Human Papillomavirus Knowledge and Vaccine Status among University Students: How Have Health Care Providers Influenced the Vaccine Decision? [dissertation]. Oklahoma State University; 2021. https://www.proquest.com/openview/267b060238d5866aba1241ad0115ac30/1.pdf
26. Marlow LAV, Waller J, Wardle J. The impact of human papillomavirus information on perceived risk of cervical cancer. Cancer Epidemiology, Biomarkers & Prevention. 2009;18(2):373-376. doi:10.1158/1055-9965.EPI-08-0357
27. Nadarzynski T, Waller J, Robb KA, Marlow LAV. Perceived risk of cervical cancer among pre-screening age women (18–24 years): the impact of information about cervical cancer risk factors and the causal role of HPV. Sex Transm Infect. 2012;88(6):400-406. doi:10.1136/sextrans-2012-050482
28. Waller J, Ostini R, Marlow LAV, McCaffery K, Zimet G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev Med. 2013;56(1):35-40. doi:10.1016/j.ypmed.2012.10.028
29. Richards K, Catalano HP, Hawkins KH. An analysis of unvaccinated college students’ HPV and HPV vaccine knowledge and preferred information source. Discourse: The Journal of the SCASD. 2019;5(4). Accessed February 26, 2025. https://openprairie.sdstate.edu/discoursejournal/vol5/iss1/4?utm_source=openprairie.sdstate.edu%2Fdiscoursejournal%2Fvol5%2Fiss1%2F4
30. Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the Health Belief Model and Theory of Planned Behavior. Ann Behav Med. 2012;44(2):171-180. doi:10.1007/s12160-012-9366-5
31. Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85-89. doi:10.1016/j.copsyc.2015.03.012
32. Cocchio S, Bertoncello C, Baldovin T, et al. Awareness of HPV and drivers of HPV vaccine uptake among university students: A quantitative, cross-sectional study. Health Soc Care Community. 2020;28(5):1514-1524. doi:10.1111/hsc.12974
33. American Society for Microbiology. HPV diagnostics, vaccines and preventive health strategies. March 22, 2023. Accessed February 5, 2025. https://asm.org:443/Articles/2023/March/HPV-Diagnostics,-Vaccines-and-Preventive-Health-St
34. Oh NL, Biddell CB, Rhodes BE, Brewer NT. Provider communication and HPV vaccine uptake: a meta-analysis and systematic review. Prev Med. 2021;148:106554. doi:10.1016/j.ypmed.2021.106554
35. Kong WY, Bustamante G, Pallotto IK, et al. Disparities in healthcare providers’ recommendation of HPV vaccination for U.S. adolescents: a systematic review. Cancer Epidemiol Biomarkers Prev. 2021;30(11):1981-1992. doi:10.1158/1055-9965.EPI-21-0733
36. Wu CF, Highfield L, Swint JM, Lairson DR. Provider-based HPV vaccine promotion interventions: A meta-analysis. Pediatrics. 2023;151(5):e2022058029. doi:10.1542/peds.2022-058029
37. Freudenthaler T, Elbon A, Schumacher K. Understanding how health care provider recommendations and messaging strategies influence HPV vaccine uptake: A study of undergraduate student perspectives. Oklahoma State Medical Proceedings. 2021;5(2). https://okstatemedicalproceedings.com/index.php/OSMP/article/view/158