WHOOPTM: Unleashing the Benefits of a Fitness Tracker for Resident Wellness
Rachael Cobbs, DO, Department of Internal Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma.
Jennifer Briggs, DO, Department of Emergency Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma.
Derek Srouji, DO, Department of Internal Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma.
Joshua Burton, DO, Department of Emergency Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma.
Katherine Cook, DO, Department of Internal Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma.
Mousumi Som, DO, Designated Institutional Official for Oklahoma State University, Department of Internal Medicine at Oklahoma State University Center for Health Sciences in
Tulsa, Oklahoma. ORCID: 0009-0000-9070-1182
Kelly Murray, PharmD, Department of Emergency Medicine at Oklahoma State University Center for Health Sciences in Tulsa, Oklahoma. ORCID: 0000-0002-8090-2156
ABSTRACT
Background: Just as it is difficult to define stress and burnout with an objective measure, stress-reducing strategies and behavioral modification techniques are also challenging to compare due to lack of objectivity. Heart rate variability (HRV) is a metric that shows promise quantitatively measuring stress and predicting burnout.
Objective: We hypothesize that the wearable device technology, WHOOPTM, will provide objective data that may enhance resident wellness.
Methods: A narrative review was conducted during the years 2020-2021 using the PubMed electronic database. Data regarding HRV was reviewed to analyze wearable devices such as the WHOOPTM as a measurement of resident stress levels and risk of burnout.
Results: Sleep, exercise, and alcohol consumption are factors that demonstrate stress-associated variation in HRV. Existing neurobiological evidence supports HRV as an objective means to assess physician stress levels. Furthermore, HRV is the metric of choice for WHOOPTM devices for measurement of strain and recovery time as affected by these factors.
Conclusion: HRV is an objective way to quantify stress, which could be used to develop screening tools for resident burnout. The WHOOP™ device provides real time data on sleep, exercise, and alcohol that residents can use to modify behavior thus promoting healthier lifestyles.
INTRODUCTION
Physician burnout is an unfortunate and increasing occurrence. In 2009, Ishak, et al. determined that 27-75% of residents experience burnout throughout their residency depending on their specialty1. Several factors have been found to contribute to feelings of stress and burnout, including lack of exercise, lack of sleep, and increased alcohol consumption. Burnout is often described in dichotomous or qualitative terms, making it hard to predict and monitor improvement. Use of reliable and trackable metrics grading the impact stress has on the body can theoretically empower residents to improve their wellness and guide strategies on stress reduction.
First, we discuss the available literature regarding heart rate variability (HRV), a well-researched metric that provides quantitative evidence of stress endured by the body2. Second, we review modifiable activities contributing to stress including exercise, alcohol consumption, and sleep, and the individual impact they have on HRV. Finally, we discuss the application of wearable technology, such as WHOOPTM, that monitors your sleep, strain, recovery and stress, which may significantly modify stress patterns, amplify productivity, and enhance the overall wellness of the resident physician. The wearable device specifically calculates biometric data of an individual’s recovery on a scale of 0 to 100%. The device measures HRV, resting heart rate, respiratory rate, oxygen saturation, sleep performance and skin temperature to determine the body’s adaptation to physiological and psychological stress.3
The purpose of this narrative review is to discuss the impact stress has on the body via HRV, as demonstrated by varying patterns of sleep, exercise, and alcohol consumption. Extrapolation of this data was used to theorize that wearable devices such as WHOOPTM can be used to objectively track resident stress levels and risk of burnout.
METHODS
This theoretical, integrative narrative review discusses an innovative approach using the WHOOPTM device to better quantify resident burnout and provide a practical solution to challenges identifying burnout in graduate medical education. The literature search took place from August 2020 to October 2021, with article reviews and manuscript synthesis taking place in 2022. English language articles published prior to October 2021 were individually collected and screened by study authors for inclusivity. PubMed was used to access literature databases and functioned as the primary search engine. Resources used for primary data collection included a broad range of peer-reviewed articles, cited references, journals, and databases. Keywords included heart rate variability, wearable devices, burnout, and stress. A secondary search method was performed using the obtained articles through these keyword searches and review of the references.
DISCUSSION
The intrigue in the role of HRV and its connections to parasympathetic and sympathetic activity have long been of interest to researchers. HRV characterizes the early effects on the heart and the imbalance between the sympathetic and the vagal systems. The deleterious impact of HRV specifically on the vagal tone of the body has been linked to increased morbidity and mortality. Perceived work stress has repeatedly been shown to be associated with increased incidence of coronary heart disease4. The following studies review HRV in student, resident, and attending physicians.
Kaegi et al. recruited 17 pediatric and anesthesia residents who underwent simulation-based training where each physician participated in a scenario simulating a medical emergency in their respective fields. They were all monitored with continuous ambulatory EKG monitoring. The EKGs were analyzed for absolute heart rate (HR) and HRV. Power spectral analysis revealed a significant increase in low frequency (LF) power, a marker of sympathetic activity and a concomitant decrease in high frequency (HF) power, a measurement of vagal activity. The LF/HF ratio, used to reflect sympathetic modulation, revealed a significant increase with stress but no significant change between minimum HR. The conclusions of this study showed a mentally stressful environment seemed to increase sympathetic activity as evidenced by an increase in LF power while also resulting in a diminution of vagal activity as seen by the decrease in HF power. HRV was concluded to be a useful tool in assessing response in stressful environments5.
Lucini et al. enrolled 30 healthy, nonsmoking, medical students and assessed autonomic involvement in two different scenarios that included 30-60 minutes before a university examination and a second time (control day) three months post-exam, separated from study routines. Data analysis was conducted incorporating spectral analysis on the systolic arterial pressure (SAP). The results of this study demonstrated that the RR interval, time measurement between two successive heartbeat intervals, was significantly smaller, whereas SAP was significantly more elevated during the day of increased stress compared with the control day. The day of increased stress was characterized by significantly higher values of low frequency RR and of LF/HF in contrast, high frequency RR was significantly smaller. These results signify an overall increase in arterial pressure. The conclusions of this study suggested that moderate real-life stressors raise resting SAP and induce important humoral changes by activating hypothalamic-pituitary-axis and altering cytokine profiles. These stress response changes led to an overall elevation in systolic pressure and a more variable HR6.
Weenk et al, conducted an explorative study looking at the impact of stress metrics as defined by components of the power spectral analysis for both attendings and residents during surgery. HRV metrics were recorded using a smart patch that was attached to the attendings/\ and residents during surgery and compared these same metrics during non-surgical daily activities of these same study participants. Stress measurement outcomes demonstrated a 64% increase in the LF/HF ratio when monitoring during an operation as compared to non-surgical daily activities. The study concluded that stress monitoring revealed significant HRV during surgeries demonstrating the role of HRV being an objective metric for stress response7.
Reviewing these studies regarding stress-associated variation in HRV and existing neurobiological evidence favors HRV as an objective means to assess the physiological response a resident physician may endure during their training. Furthermore, HRV is the metric of choice for WHOOPTM devices for measurement of strain and recovery time as affected by factors such as sleep, exercise, and alcohol intake. We propose WHOOPTM could pioneer analysis through HRV and subsequently drive improvements in the physician’s mental and physical health. The following sections discuss the impact of exercise, sleep deprivation, and alcohol consumption on resident stress and burnout.
Contribution of exercise
Although sleep variability and decreased physical activity are known precipitating factors for major depression, a lack of objective real-time information has limited our understanding of how factors such as inactivity and lack of exercise have contributed to resident mental health. Efforts have been made to acquire more prospective data to provide critical insights into physicians’ behaviors and the effect these have on the workplace environment.
Stress in medical education including residency training has been well-documented. Using an online questionnaire, 168 first-year family medicine residents completed standardized measures exploring perceived stress, depression, satisfaction with life, and burnout which revealed 23.0% who scored consistent with depression. This study also showed that residents with high levels of physical activity had lower levels of depression, depersonalization, and emotional exhaustion as well as a tendency towards increased satisfaction with life8.
Williams et al. investigated the barriers that may be present in prohibiting residents from achieving higher rates of exercise. Three focus groups with first-year residents, senior residents and attending physicians at the University of Missouri Department of Family and Community Medicine found that during inpatient rotations, 0% of residents compared to 18.4% of attendings exercised more than 150 minutes/week. In addition, 6.9% of residents exercised more than 150 minutes/week during non-inpatient rotations compared to 25.0% of attendings during the same time interval. Lack of time was reported as a major barrier by residents9. The study suggests that decreasing barriers and promoting methods for exercise has the potential to improve resident well-being by ensuring more consistent physical exercise.
Kalmbach et al conducted a prospective longitudinal study that examined 33 first-year residents who consented to provide objective data from FitBit™ technology from two months pre-internship through the first six months of internship. Results of the study showed that physical activity decreased by 11.5% after transitioning to internship. First-year residents also reported a subjective worsening of their mood when they were less active10. This leads us to believe that a reduction in physical activity may increase the risk for negative mood outcomes.
Physical activity during residency is an underestimated area that warrants more focused attention for its role in stress and physiological well-being. By providing the means to monitor objective data produced from physical activity, wearable technology may help improve resident well-being.
Contribution of sleep
Sleep deprivation occurs when an individual fails to get enough sleep. In 2019, 35% of U.S. adults have been reported to sleep less than seven hours over a 24-hour period, which is below the recommended duration of sleep according to the National Sleep Foundation11. Resident physicians are particularly vulnerable due to their work responsibilities, and sleep deprivation in residency typically occurs secondary to voluntary behaviors, personal obligations, or work hours. Because of this the Accreditation Council for Graduate Medical Education (ACGME) includes guidelines for residency programs to protect against the dangers of sleep deprivation (table 1). Sleep deprivation within the medical field increases the risk of medical errors and poor physician health12. Therefore, sleep deprivation among resident physicians should be explored to better understand its relationship to poor medical outcomes, wellness, and HRV.
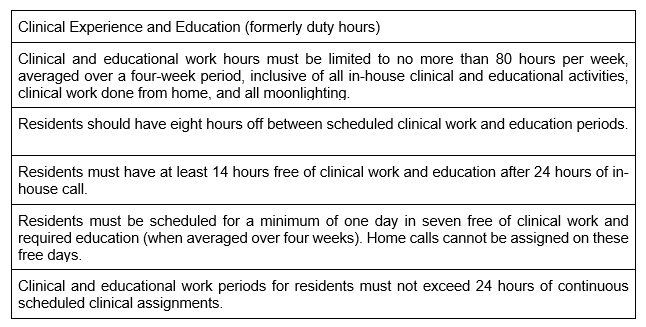
Table 1: Clinical Experience and Education (Formerly duty hours). ACGME Common Program
Requirements Section VI with Background and Intent. (Summary of Changes to ACGME Common Program Requirements Section VI. (n.d.). Retrieved from https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements/Summary-of-Proposed-Changes-to-ACGMECommon-Program-Requirements-Section-VI)
In a nationwide study of 2,737 U.S. first-year residents, 16% of significant medical errors and 1.6% of preventable adverse events were reported in conjunction with extended duration work shifts (EDWS). Additional results revealed significant increases in attentional failures including falling asleep during surgery, examining a patient, attending lectures, and on rounds occurred in conjunction with increasing the number of EDWS13. Despite ACGME duty hour restrictions (table 1), residents continue to suffer from sleep deprivation. In a 2019 article, more than four hours of actual sleep was required to significantly decrease the amount of attention related errors when compared to no overnight sleep. Only 8% of analyzed residents obtained more than four hours of actual sleep during an EDWS14.
As mentioned above, the Kalmbach study correlated sleep deprivation to worsening mood. When first-year residents lost 2 hours and 48 minutes of sleep per week, mood decreased by 7.5%10.
Though these studies give insight into the current environment of residents and potential harms that may result due to sleep deprivation, could HRV serve as an early indication for trouble? There have been several investigations on how sleep deprivation may impact HRV. In an internal medicine residency program, otherwise healthy residents were studied over a 26 hour on-call period revealing an increase in sympathetic modulation as recorded by low frequency HRV15. In another study, 40 hours of continuous sleep deprivation in otherwise healthy adult males revealed low frequency HRV data demonstrating significant increases in sympathetic activity16. Among anesthesiology residents, increased stress from anticipating an upcoming night shift was associated with decreased parasympathetic activity through assessment of high frequency HRV17.
At the University of Arizona, the WHOOPTM device was compared to the gold-standard
polysomnography to assess its reliability in measuring sleep quantity and sleep fragmentation. The WHOOPTM devices’ ability to measure various sleep stages was considered excellent through the use of the interclass correlation coefficient analysis under blinded conditions18. Such wearable technology that accurately measures HRV and sleep may be a promising intervention in promoting wellness to residents.
Contribution of alcohol
Approximately 10 to 15% of all healthcare professionals will misuse alcohol during their career19 Problematic use of alcohol in physicians has also increased over time, from 16.3% in 2006-2010 to 26.8% in 2017-202020. Alcohol has a profound influence on behavior, sleep and recovery. Heavy alcohol consumption has been linked to longer times to fall asleep as well as abnormal breathing-related events during sleep, especially in those with obstructive sleep apnea21. Studies have demonstrated an increase in NREM sleep due to alcohol but a decrease in replenishing REM sleep22. For example, Sahlin et al. demonstrated a difference in sleep latency of 47 minutes versus 21 minutes in women dependent on alcohol versus a control group. Similarly, time spent in REM sleep was significantly less at 64 minutes for the alcohol dependent subjects compared to 77 minutes for the control group23. Evidence of disrupted sleep has also been shown when comparing low versus high work-demanding occupations. Workers in high-stress occupations showed an increased odds of sleep disturbance compared to low-stress occupations (OR 2.15, CI 1.29-3.58)24. High stress occupations and inadequate sleep were also found to be associated with increased alcohol dependence or abuse. An observation of Navy service members in 2017 showed the parallel effects of long work hours with frequency of alcohol use (β = .12)25.
WHOOPTM has the ability to analyze the effect of alcohol on sleep and recovery. In a small user-reported review, WHOOPTM users were shown to consume less alcohol after being made aware of alcohol’s detrimental effects on HRV and sleep. Not only could this lessen the rate of alcohol use in physicians, but this could also spark more attention to sleep hygiene in the residents suffering from burnout. A study of 115 internal medicine residents analyzed the relationship between stress and burnout highlighted inadequate sleep in 41% and inadequate leisure time in 42% of residents who met criteria for burnout. Furthermore, approximately half of residents who met criteria for burnout reported at least one error in patient care monthly and almost a third reported at least one error weekly26. With the high prevalence of alcohol use in the medical field, self-monitoring of alcohol intake and sleep hygiene may have a positive impact on behaviors that would promote increased resiliency.
How wearable devices show evidence towards benefit when you track these markers
The Stanford 2020 Health Trends reported that 50% of residents and 44% of attending physicians own wearable technology27. These devices are designed to ease convenience of communications, perform various medical assessments, and track physical activity. As many as 71% of these users review and apply this data when making personal health care decisions27. Some devices are engineered with very specific health care metrics in mind. For example, the Empatica wrist device can sense and quantify autonomic dysfunction patterns found during generalized tonic-clonic seizures. In a review compiled by Regalia et al., performance in inpatient and outpatient settings demonstrates a sensitivity of >92% and false alarm rate of 0.2-1 false alarms per day for automated detection of generalized tonic-clonic seizures28. Sensitivities and false alarm rates were most impacted by motion, with greatest accuracy during periods of rest. Similar concern regarding accuracy of HR monitoring in smart watches and fitness trackers has been expressed. More than 400 fitness trackers and smart watches have been marketed since 2011, the vast majority dependent on photoplethysmogram (PPG) technology for HR analysis29.
Accuracy and reliability of PPG technology for HR monitoring and analysis has been reviewed in a diverse number of settings, including cardiac rehabs, hospitals, and home30-32. Apple conducted a survey on 419,297 participants who wore the Apple Watch, assessing for notification of pulse irregularities. Among those who met inclusion criteria, watch notifications of irregular pulse were concordant with atrial fibrillation 84% of the time (95% CI, 76-92)33. Use of this technology to detect atrial fibrillation was later validated in a single-center tertiary care facility, demonstrating a mean difference in RR interval of 3.83 + 113.54 ms, with a correlation coefficient of 0.7934.34
Use of a wearable device, such as a smartwatch or fitness tracker, has been shown to be feasible in the clinical environment, and may influence personal habits such as sleep and exercise. Because the WHOOPTM device has been widely adopted by many athletes to assess stress, strain, and recovery, one can assume members of the medical community may also benefit from the information it may provide.
Effect of burnout
Over the past decade, increasing emphasis has been placed on physician wellness and burnout rates. Resident burnout prevalence rates as high as 47-70% have been reported in the literature35. Residents were found to be six times less likely to report fulfillment in work or school, and 13 times less likely to exhibit overall career satisfaction in comparison to medical students36. High stress, chronic sleep deprivation, social isolation, and increasing work burden predisposes physicians to depression and feelings of depersonalization37-39. Validated survey tools such as the Maslach Burnout Index (MBI), Patient Health Questionnaire (PHQ), Generalized Anxiety Disorder Questionnaire (GAD), and Epworth Sleepiness Scale (ESS) have been utilized to identify those at risk for burnout.40-41 Papp et al. evaluated sleep habits in 149 multi-disciplinary residents, reporting 84% had an EPS Score of 11 or greater, a range where clinical intervention is needed39. There is data to suggest that higher rates of burnout correspond with worsened in-training examination scores42-43. In addition to poor health and performance, the consequences of sleep deprivation, depression, and increased work hours appear to correlate with higher rates of medical errors37,44. Sturm et al. suggested that perceptions of increased work-related stress and patient care-related burnout are associated with increased readmission rates and increased patient morbidity 38. In a study of 6586 participants, 691 reported a self-perceived major medical error in the previous three months, 9.8% of which resulted in significant morbidity or mortality. This cohort of participants was also found to report higher levels of fatigue and symptoms of burnout 45.
Limitations
Though promising data exists, using biometric data to quantify resident wellness by way of exercise, alcohol use, and sleep may have its limitations. For example, residents and physicians may have changes in HRV based on the time of day a rotation occurs, i.e. night shifts that may impact sleep patterns as well as rotation type (inpatient vs outpatient). Also, wearable devices in general may have limitations in data quality and balanced estimations, such as standardization of sensor reliability and application to human contextual information. In addition to these limitations, the lifestyle of a resident will likely be different than an elite athlete and extrapolations of data may not be consistent between the two. Balanced estimations are important to consider in the resident population as broad interpretation of data may either overestimate or over-predict burnout when metrics may be more closely related to overall poor lifestyle choices.46 Lastly, consideration of the short period in which data was reviewed serves as a limitation. As devices continue to advance and become more accessible, data should be continuously reviewed for additional information that would lend to the validity of using wearable devices to help in monitoring residents' overall health.
All identified and possible limitations support the need for further research of wearable devices in physicians to determine correlation and applicability to wellness and burnout. We propose WHOOPTM could facilitate resident-directed awareness of independent behaviors that contribute to HRV. This could identify modifiable habits that would result in longer-term changes in mental and physical health and ultimately the ability to perform optimal patient care.
CONCLUSION
Despite the use of routine surveys and adjustments to resident physician work hours, burnout continues to be a topic of discussion. Resident burnout identification and prevention strategies are necessary to facilitate an environment of patient safety and resident well-being. Assessments of HRV can provide real time, objective insight into the personal wellness of physicians in training. By using wearable devices such as WHOOP™, real time data on sleep, exercise, and alcohol effects can be displayed to the resident via HRV to promote healthier lifestyles. We believe the long-term effects of improved resident well-being likely extend far beyond just resident satisfaction. WHOOP™ will positively impact future physicians by empowering them to pivot towards mechanisms that allow for self-identified resiliency strategies through daily monitoring of individual health. The next steps of researching this topic would focus on using the innovative WHOOP™ band technology to evaluate and validate these claims in future studies.
REFERENCES
1. Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242.
2. Marques AH, Silverman MN, Sternberg EM. Evaluation of stress systems by applying noninvasive methodologies: measurements of neuroimmune biomarkers in the sweat, heart rate variability and salivary cortisol. Neuroimmunomodulation. 2010;17(3):205-208.
3. What WHOOP TM Measures. WHOOP TM. Updated unknown date. Accessed March 6, 2024. https://www.whoop.com/us/en/the-data/
4. Tsuji H, Venditti FJ Jr, Manders ES, Evans JC, Larson MG, Feldman CL, et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation. 1994;90(2):878-883.
5. Kaegi DM, Halamek LP, Van Hare GF, Howard SK, Dubin AM. Effect of Mental Stress on Heart Rate Variability: Validation of Simulated Operating and Delivery Room Training Modules. Pediatr Res. 1999;45(7):77-77.
6. Lucini D, Norbiato G, Clerici M, Pagani M. Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension. 2002;39(1):184-188.
7. Weenk M, Alken APB, Engelen LJLPG, Bredie SJH, van de Belt TH, van Goor H. Stress measurement in surgeons and residents using a smart patch. Am J Surg. 2018;216(2):361-368.
8. Lebensohn P, Dodds S, Benn R, Brooks AJ, Birch M. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541-549.
9. Williams AS, Williams CD, Cronk NJ, Kruse RL, Ringdahl EN, Koopman RJ. Understanding the Exercise Habits of Residents and Attending Physicians. Fam Med. 2015;47(2):118-123.
10. Kalmbach DA, Fang Y, Arnedt JT, Cochran AL, Deldin PJ, Kaplin AI, et al. Effects of Sleep, Physical Activity, and Shift Work on Daily Mood: a Prospective Mobile Monitoring Study of Medical Interns. J Gen Intern Med. 2018;33(6):914-920.
11. Bandyopadhyay A, Sigua NL. What Is Sleep Deprivation? Am J Respir Crit Care Med. 2019;199(6):P11-P12.
12. Wong LR, Flynn-Evans E, Ruskin KJ. Fatigue Risk Management: The Impact of Anesthesiology Residents' Work Schedules on Job Performance and a Review of Potential Countermeasures. Anesth Analg. 2018;126(4):1340-1348.
13. Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487.
14. St Hilaire MA, Anderson C, Anwar J, Sullivan JP, Cade BE, Flynn-Evans EE, et al. Brief (<4 hr) sleep episodes are insufficient for restoring performance in first-year resident physicians working overnight extended-duration work shifts. Sleep. 2019;42(5).
15. Tobaldini E, Cogliati C, Fiorelli EM, Nunziata V, Wu MA, Prado M, et al. One night on-call: sleep deprivation affects cardiac autonomic control and inflammation in physicians. Eur J Intern Med. 2013;24(7):664-670.
16. Sauvet F, Leftheriotis G, Gomez-Merino D, Langrume C, Drogou C, Van Beers P, et al. Effect of acute sleep deprivation on vascular function in healthy subjects. J Appl Physiol (1985). 2010 Jan;108(1):68-75.
17. Wang ML, Lin PL, Huang CH, Huang HH. Decreased Parasympathetic Activity of Heart Rate Variability During Anticipation of Night Duty in Anesthesiology Residents. Anesth Analg. 2018;126(3):1013-1018.
18. Berryhill S, Morton CJ, Dean A, Berryhill A, Provencio-Dean N, Patel SI, Estep L, et al. Effect of wearables on sleep in healthy individuals: a randomized crossover trial and validation study. J Clin Sleep Med. 2020 May 15;16(5):775-783.
19. Baldisseri MR. Impaired healthcare professional. Crit Care Med. 2007;35(2 Suppl):S106-16.
20. Wilson J, Tanuseputro P, Myran DT, et al. Characterization of problematic alcohol use among physicians: A systematic review. JAMA Netw Open. 2022;5(12):e2244679.
21. He S, Hasler BP, Chakravorty S. Alcohol and sleep-related problems. Curr Opin Psychol. 2019;30:117-122.
22. Thakkar MM, Sharma R, Sahota P. Alcohol disrupts sleep homeostasis. Alcohol. 2015;49(4):299-310.
23. Sahlin C, Franklin KA, Stenlund H, Lindberg E. Sleep in women: Normal values for sleep stages and position and the effect of age, obesity, sleep apnea, smoking, alcohol and hypertension. Sleep Med. 2009;10(9):1025-1030.
24. Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours: A cross-sectional study. J Psychosom Res. 2002;53(3):741-748.
25. Bravo AJ, Kelley ML, Hollis BF. Work stressors, sleep quality, and alcohol-related problems across deployment: A parallel process latent growth modeling approach among Navy members. Stress Health. 2017;33(4):339-347.
26. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358-367.
27. The Rise of the Data-Driven Physician. Stanford Medicine News Center. https://med.stanford.edu/content/dam/sm/school/documents/Health-Trends-Report/Stanford%20Medicine%20Health%20Trends%20Report%202020.pdf. Published January 9, 2020. Accessed October 1, 2020.
28. Regalia G, Onorati F, Lai M, Caborni C, Picard RW. Multimodal wrist-worn devices for seizure detection and advancing research: Focus on the Empatica wristbands. Epilepsy Res. 2019 Jul;153:79-82.
29. Henriksen A, Haugen Mikalsen M, Woldaregay AZ, Muzny M, Hartvigsen G, Hopstock LA, et al. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J Med Internet Res. 2018 Mar 22;20(3):e110. doi: 10.2196/jmir.9157.
30. Falter M, Budts W, Goetschalckx K, Cornelissen V, Buys R. Accuracy of Apple Watch Measurements for Heart Rate and Energy Expenditure in Patients With Cardiovascular Disease: Cross-Sectional Study. JMIR Mhealth Uhealth. 2019 Mar 19;7(3):e11889. doi: 10.2196/11889.
31. Hettiarachchi IT, Hanoun S, Nahavandi D, Nahavandi S. Validation of Polar OH1 optical heart rate sensor for moderate and high intensity physical activities. PLoS One. 2019 May 23;14(5):e0217288. doi: 10.1371/journal.pone.0217288.
32. Jenks S, Frank Peacock W, Cornelius AP, Shafer S, Pillow MT, Rayasam SS. Heart rate and heart rate variability in emergency medicine. Am J Emerg Med. 2020 Jul;38(7):1335-1339.
33. Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al; Apple Heart Study Investigators. Large-Scale Assessment of a Smartwatch to Identify Atrial Fibrillation. N Engl J Med. 2019 Nov 14;381(20):1909-1917.
34. Saghir N, Aggarwal A, Soneji N, Valencia V, Rodgers G, Kurian T. A comparison of manual electrocardiographic interval and waveform analysis in lead 1 of 12-lead ECG and Apple Watch ECG: A validation study. Cardiovasc Digit Health J. 2020 Aug 26;1(1):30-36.
35. Spiotta AM, Fargen KM, Patel S, Larrew T, Turner RD. Impact of a Residency-Integrated Wellness Program on Resident Mental Health, Sleepiness, and Quality of Life. Neurosurgery. 2019 Feb 1;84(2):341-346. doi: 10.1093/neuros/nyy112. Erratum in: Neurosurgery. 2019 Jun 1;84(6):E334-E344.
36. Hull SK, DiLalla LF, Dorsey JK. Prevalence of health-related behaviors among physicians and medical trainees. Acad Psychiatry. 2008 Jan-Feb;32(1):31-8.
37. Kalmbach DA, Arnedt JT, Song PX, Guille C, Sen S. Sleep Disturbance and Short Sleep as Risk Factors for Depression and Perceived Medical Errors in First-Year Residents. Sleep. 2017 Mar 1;40(3):zsw073. doi: 10.1093/sleep/zsw073.
38. Sturm H, Rieger MA, Martus P, Ueding E, Wagner A, Holderried M, et al; WorkSafeMed Consortium. Do perceived working conditions and patient safety culture correlate with objective workload and patient outcomes: A cross-sectional explorative study from a German university hospital. PLoS One. 2019 Jan 4;14(1):e0209487. doi: 10.1371/journal.pone.0209487.
39. Papp KK, Stoller EP, Sage P, Aikens JE, Owens J, Avidan A, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2004 May;79(5):394-406.
40. Lin CY, Alimoradi Z, Griffiths MD, Pakpour AH. Psychometric properties of the Maslach Burnout Inventory for Medical Personnel (MBI-HSS-MP). Heliyon. 2022 Feb 1;8(2):e08868.
41. National Academy of Medicine. Valid and Reliable Survey Instruments to Measure Burnout, Well-Being, and Other Work-Related Dimensions. Updated unknown date. Accessed March 6, 2024. https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions/
42. West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011 Sep 7;306(9):952-60.
43. Strauss EJ, Markus DH, Kingery MT, Zuckerman J, Egol KA. Orthopaedic Resident Burnout Is Associated with Poor In-Training Examination Performance. J Bone Joint Surg Am. 2019 Oct 2;101(19):e102. doi: 10.2106/JBJS.18.00979.
44. Hewitt DB, Ellis RJ, Chung JW, Cheung EO, Moskowitz JT, Huang R, et al. Association of Surgical Resident Wellness With Medical Errors and Patient Outcomes. Ann Surg. 2021 Aug 1;274(2):396-402.
45. Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018 Nov;93(11):1571-1580.
46. Canali S, Schiaffonati V, Aliverti A. Challenges and recommendations for wearable devices in digital health: Data quality, interoperability, health equity, fairness. PLOS Digit Health. 2022 Oct 13;1(10):e0000104.