Doxycycline vs. Penicillin G Benzathine for the Treatment of Syphilis in Patients with HIV
A. Cole Eichelberger, PharmD, BCPS, AAHIVP, Oklahoma State University Medical Center, Department of Pharmacy
Isaac D. Nichols, PharmD, BCPS ,Oklahoma State University Medical Center, Department of Pharmacy
Bryan A. Bozell, PharmD, BCPS, AAHIVP, Oklahoma State University Center for Health Sciences, Department of Internal Medicine
Corresponding Author:
Clinical Pharmacist
Department of Pharmacy
Address – 5079 S. 136th East Ave. Apt. 221 Tulsa, OK 74134
Email Address – aceichelberger@osumc.net
Conflicts of Interest: The authors involved in this project have no competing financial interests to disclose
INTRODUCTION
Syphilis is a sexually transmitted infection that can cause significant health complications if left untreated.1 It is caused by the spirochete Treponema pallidum, a bacterium that is difficult to culture and genetically manipulate.1 Transmission occurs through sexual contact, perinatally, or via direct exposure to a syphilitic chancre.2 If untreated, syphilis progresses through multiple stages, including primary, secondary, tertiary, latent, cardiovascular, gummatous, and neurosyphilis.
Due to its elusive nature, syphilis diagnosis requires specialized testing. Direct detection methods, such as darkfield microscopy, can identify T. pallidum, while serologic diagnosis relies on non-treponemal tests—such as the Venereal Disease Research Laboratory (VDRL) and rapid plasma reagin (RPR) tests—alongside treponemal assays, including enzyme immunoassays (EIAs), rapid treponemal tests, and T. pallidum particle agglutination (TP-PA).2
Syphilis and HIV co-infection is a growing public health concern, particularly among men who have sex with men (MSM). Studies show that individuals with HIV are at significantly higher risk of acquiring syphilis, with co-infection rates among MSM reaching up to 50% in some populations.3 Syphilis facilitates HIV transmission by disrupting mucosal barriers, increasing the risk of acquisition by 2-5 times, while HIV alters the natural history of syphilis, leading to faster disease progression and increased risk of neurosyphilis.4 Additionally, serologic responses to syphilis may be delayed or atypical in HIV-positive individuals, complicating diagnosis and follow-up.5
Penicillin G benzathine remains the first-line treatment for syphilis in patients with HIV, while doxycycline serves as an alternative for patients with penicillin allergies.2 Other treatment options, including ceftriaxone, azithromycin, and aqueous crystalline penicillin G, vary depending on the stage of the disease.2 For early syphilis, a single intramuscular dose of 2.4 million units of penicillin G benzathine is recommended, whereas doxycycline requires a 14-day course of 100 mg orally twice daily.2 For late-latent syphilis or cases with an unknown duration, penicillin G benzathine is administered as 2.4 million units intramuscularly once weekly for three weeks, while doxycycline is prescribed at 100 mg twice daily for 28 days.2
Several studies have evaluated doxycycline’s effectiveness in treating syphilis. In one study of 107 patients with early syphilis, serologic failure occurred in 5.5% of those treated with penicillin G benzathine and 0% of those receiving doxycycline, with no statistically significant difference between the groups.6 Likewise, a 2016 retrospective study of 118 patients utilizing doxycycline for syphilis treatment reported serological response rates of 100% in primary syphilis, 96.9% in secondary syphilis, 91.3% in early latent syphilis, and 79.2% in late latent syphilis, supporting this agent as an effective alternative therapy.7 Similarly, another study analyzing 601 cases of early syphilis found no significant difference in serological response rates between doxycycline (69.5% at six months, 92.4% at twelve months) and penicillin G benzathine (75.0% at six months, 96.2% at twelve months).8
Despite these findings, data on doxycycline’s efficacy in patients with syphilis with concurrent HIV infection remain limited. Since syphilis increases the risk of HIV acquisition and may lead to more severe neurological complications in individuals living with HIV, ensuring effective treatment in this population is crucial. This study aimed to evaluate the effectiveness of doxycycline in treating syphilis among HIV-positive patients, contributing to the existing body of knowledge on this alternative therapy.2
METHODS
This retrospective cohort chart review was conducted from October 10, 2020, to July 31, 2022, at Oklahoma State University Internal Medicine Specialty Services (OSU IMSS), an urban outpatient primary care clinic specializing in HIV care and serving over 1,300 patients annually. Encounters were identified using International Classification of Disease (ICD) codes for syphilis. Eligible patients had to receive either penicillin G benzathine or doxycycline.
Patient charts were included if individuals were ≥18 years old, diagnosed with HIV, had new or recurrent syphilis, and had a documented prescription for doxycycline or penicillin G benzathine. Exclusion criteria included age <18 years, neurosyphilis at the time of treatment, pregnancy, or insufficient data to assess treatment response.
The primary endpoint was syphilis resolution, defined as a four-fold decrease in RPR at 12 months post-treatment. Secondary endpoints included co-infection rates and reported adverse reactions. An information technology specialist at OSU IMSS generated a list of patients with syphilis, HIV, and documented prescriptions for the specified treatments. The research team then compiled the data in Microsoft Excel. Patients were categorized into doxycycline or penicillin G benzathine treatment groups. Infection resolution was recorded dichotomously as "0" (not resolved) or "1" (resolved). Fisher’s exact test was used for primary endpoint analysis, with descriptive statistics applied to all outcomes. A two-sided alpha level of 0.05 was set, and statistical analysis was conducted in Microsoft Excel. Power was determined post-hoc using G*Power given alpha, sample size, and effect size.
This study was deemed exempt by the institutional review board at the study facility prior to data collection and analysis.
RESULTS
A total of 370 patient encounters were identified for chart review. Of these, 236 were excluded, primarily due to insufficient data to assess treatment response, often resulting from recent treatment or lack of follow-up. This left 134 encounters for analysis, with 113 patients in the penicillin G benzathine group and 21 in the doxycycline group.
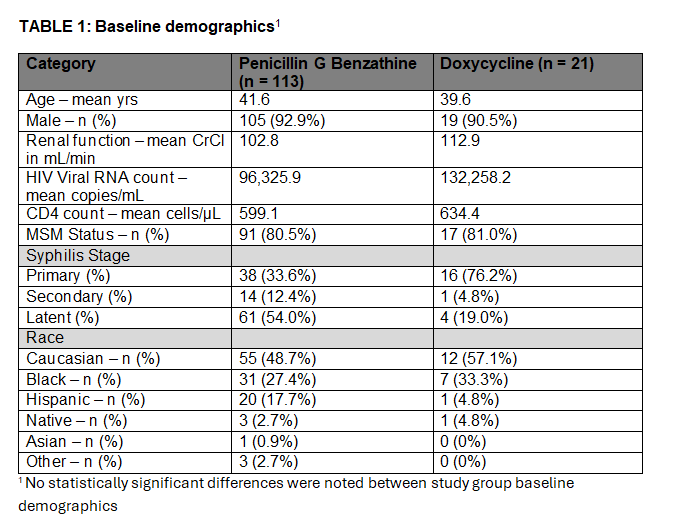
The average age was 41.6 years in the penicillin G benzathine group and 39.6 years in the doxycycline group. Most patients were male (92.9% in the penicillin group, 90.5% in the doxycycline group), with a high proportion identifying as MSM (80.5% and 81%, respectively). The mean HIV RNA count was 96,325 copies/mL in the penicillin group and 132,258 copies/mL in the doxycycline group. Mean CD4 count was 599 cells/µL in the penicillin group and 634 cells/µL in the doxycycline group. Syphilis staging differed between groups: in the penicillin arm, 61 patients had latent syphilis, 14 had secondary syphilis, and 38 had primary syphilis. In the doxycycline arm, there were 4 cases of latent syphilis, 1 case of secondary syphilis, and 16 cases of primary syphilis. Baseline demographics are detailed in Table 1.
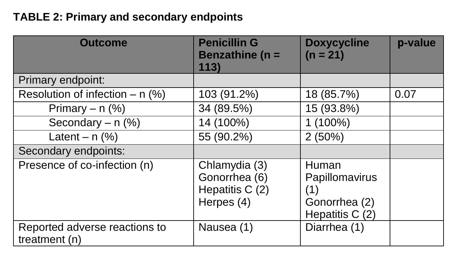
The primary outcome—resolution of syphilis infection—was achieved in 103/113 (91.6%) patients treated with penicillin G benzathine and 18/21 (85.7%) treated with doxycycline (p = 0.07; OR 1.72; CI 0.43-6.86). Within the penicillin group, resolution rates were 89.5% (34/38) for primary syphilis, 100% (14/14) for secondary syphilis, and 90.2% (55/61) for latent syphilis. In the doxycycline group, resolution occurred in 93.8% (15/16) of primary syphilis cases, 100% (1/1) of secondary syphilis cases, and 50% (2/4) of latent syphilis cases.
Co-infections were identified in 15 patients in the penicillin group and 5 in the doxycycline group. Among those treated with penicillin, gonorrhea (6 cases) was the most prevalent, while gonorrhea (2 cases) and hepatitis C (2 cases) were the most reported co-infections in the doxycycline group. Reported adverse effects were minimal, with one case of nausea in the penicillin group and one case of diarrhea in the doxycycline group. All clinical outcomes are summarized in Table 2.
DISCUSSION
Evaluating the efficacy of doxycycline in treating syphilis among HIV-positive individuals is critical, given the limited alternative treatments available for penicillin-allergic patients. This study compared doxycycline to the standard therapy, penicillin G benzathine, in an HIV-positive population and found no statistically significant difference in treatment success between the two groups (p = 0.07). However, numerical differences in resolution rates and key study limitations highlight the need for further investigation in this population.
While penicillin G benzathine remains the first-line treatment for syphilis, doxycycline is commonly used as an alternative therapy, particularly for patients with contraindications to penicillin. In this study, the syphilis resolution rate was slightly higher in the penicillin group (91.6%) compared to the doxycycline group (85.7%), which aligns with previous research suggesting penicillin's superior efficacy in syphilis treatment.9 However, the sample size disparity between groups (113 vs. 21 patients, respectively) may have limited the ability to detect a statistically significant difference. Additionally, the difference in syphilis staging between treatment arms—where a larger proportion of doxycycline-treated patients had primary syphilis, while more penicillin-treated patients had latent syphilis—may have contributed to the observed outcome differences. Given that early-stage syphilis tends to respond more favorably to treatment, this imbalance could have influenced the resolution rates.
Another key finding was that co-infection with other sexually transmitted infections (STIs) did not appear to affect syphilis treatment outcomes. This is particularly relevant, as HIV-positive individuals are at increased risk for multiple STIs, which may complicate disease management.10 The presence of co-infections such as gonorrhea, chlamydia, hepatitis C, and herpes did not show a clear correlation with treatment success, suggesting that doxycycline and penicillin G benzathine remain effective in this setting. However, further studies with larger sample sizes and stratification by co-infection status are warranted to confirm this observation.
Adverse effects were minimal in both treatment groups, with only one case of nausea reported in the penicillin group and one case of diarrhea in the doxycycline group. This low incidence of side effects is consistent with previous literature on the tolerability of both medications.11 However, given the retrospective nature of the study, underreporting of adverse effects is a potential limitation. Future prospective studies with standardized adverse event monitoring would provide a more accurate assessment of drug tolerability in this population.
Several limitations must be acknowledged. First, this was a retrospective single-center study, limiting both the availability of data and the generalizability of findings. The exclusion of 236 encounters, primarily due to insufficient follow-up data, may have introduced selection bias, as patients who were lost to follow-up may have had different treatment responses. Additionally, while statistical analysis suggested no significant difference between treatment groups, the study did not meet power, meaning a true difference may exist but was not detected due to the small sample size.
The imbalance in syphilis staging between treatment groups is another important confounder. Since early syphilis is typically more responsive to treatment, the higher proportion of primary syphilis cases in the doxycycline group may have contributed to the observed treatment success rates.12 A future prospective study with randomization to ensure balanced syphilis staging between treatment arms would help clarify this issue. Adherence is another important confounder in this study. Penicillin G benzathine, being administered as intramuscular injections, allows for more straightforward monitoring of patient compliance. In contrast, doxycycline requires a 14 to 28-day course of oral administration, which demands a higher level of patient adherence and may influence the observed treatment outcomes.
Finally, the potential impact of HIV disease severity on syphilis treatment response warrants further exploration. While CD4 counts and HIV viral loads were similar between groups, it remains unclear whether patients with more advanced HIV disease (e.g., CD4 < 200 cells/µL) may respond differently to syphilis treatment. Some studies suggest that lower CD4 counts may be associated with slower serologic response, though data remain inconclusive.13 Larger studies with stratification by HIV disease severity could provide further insights into this question.
This study adds to the growing body of evidence supporting doxycycline as an alternative treatment for syphilis in HIV-positive patients. While no statistically significant difference in resolution rates was observed compared to penicillin G benzathine, study limitations, including small sample size and differences in syphilis staging, suggest that additional larger, prospective, randomized studies are needed to confirm these findings. Given the importance of effective syphilis treatment in this population, further research should aim to optimize treatment strategies, particularly for those with latent syphilis or advanced HIV disease.
REFERENCES
1. Centers for Disease Control and Prevention (CDC). Syphilis among persons with HIV infection. CDC STD Treatment Guidelines. Published 2022. Accessed October 10, 2022. https://www.cdc.gov/std/treatment-guidelines/syphilis-hiv.htm
2. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Accessed September 23, 2022. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection
3. Patton ME, Su JR, Nelson R, Weinstock H. Primary and secondary syphilis—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(18):402-406.
4. Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis. 2007;44(9):1222-1228. doi:10.1086/513427
5. Ghanem KG, Erbelding EJ, Wiener ZS, Rompalo AM. Serological response to syphilis treatment in HIV-positive and HIV-negative patients attending sexually transmitted diseases clinics. Sex Transm Infect. 2008;84(2):97-101. doi:10.1136/sti.2007.026740
6. Ghanem KG, Erbelding EJ, Cheng WW, Rompalo AM. Doxycycline compared with benzathine penicillin for the treatment of early syphilis. Clin Infect Dis. 2006;42(6):e45-e49. doi:10.1086/500406
7. Dai T, Qu R, Liu J, Zhou P, Wang Q. Efficacy of doxycycline in the treatment of syphilis. Antimicrob Agents Chemother. 2016;61(1):e01092-16. Published December 27, 2016. doi:10.1128/AAC.01092-16
8. Xiao H, Liu D, Li Z, et al. Comparison of doxycycline and benzathine penicillin G for the treatment of early syphilis. Acta Dermatovenerol Croat. 2017;25(2):107-111.
9. Hook EW III, Marra CM. Syphilis in adults: Clinical manifestations and management. N Engl J Med. 1992;326(16):1060-1069. doi:10.1056/NEJM199204163261607.
10. Cohen MS, Hoffman IF, Royce RA, et al. Reduction of concentration of HIV-1 in semen after treatment of urethritis: Implications for prevention of sexual transmission of HIV-1. Lancet. 1997;349(9069):1868-1873. doi:10.1016/S0140-6736(97)02190-9.
11. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. doi:10.15585/mmwr.rr7004a1.
12. Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: A systematic review. JAMA. 2014;312(18):1905-1917. doi:10.1001/jama.2014.13259.
13. Ghanem KG, Erbelding EJ, Wiener ZS, Rompalo AM. Serological response following neurosyphilis therapy among HIV-infected and HIV-uninfected patients. Clin Infect Dis. 2005;41(3):420-426. doi:10.1086/431984.