“StudentBody” and “StudentBody+”: Research and Translational Learning and for the Student Body Through Medical Imaging
Amanda N Pennings, BA, Department of Anatomy and Cell Biology, Oklahoma State University Center for Health Sciences, Tulsa, OK
Lauren Hartsell, BS, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Tyler McKenzie, BS, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Kelcey Nees, BS, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Kaylin Ray, BS, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Ryan Emmert, BS, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Daniel Molina, BS, Oklahoma State University Center for Health Sciences, Tulsa, OK
David Ryan, BS, Oklahoma State University Center for Health Sciences, Tulsa, OK
Forrest LaFleur, MS, Pharmacology & Physiology, OSU-CHS; OSU Biomedical Imaging Center, OSU-CHS, Tulsa, OK
Bidhan Lamichhane, Ph.D., Pharmacology & Physiology, OSU-CHS; OSU Biomedical Imaging Center, OSU-CHS, Tulsa, OK
W. Kyle Simmons, Ph.D., Pharmacology & Physiology, OSU-CHS; OSU Biomedical Imaging Center, OSU-CHS, Tulsa, OK
Eric Snively, Ph.D., Department of Anatomy and Cell Biology, Oklahoma State University College of Osteopathic Medicine at the Cherokee Nation, Tahlequah, OK
Corresponding Author: Amanda Pennings. Address: 700 N Greenwood Ave, Tulsa, OK 74106. Email: amanda.nicole.pennings@okstate.edu.
Funding: The research leading to these results has received funding from the Graduate Student Research Program Support Fund, OSU Foundation, the OSU College of Osteopathic Medicine for software licenses, and OSU Biomedical Sciences startup funds to Dr. Eric Snively.
Conflict of Interest Statement: Authors have no conflict of interest to declare
Abstract
Background: Medical imaging is a cornerstone of biomedical research and clinical practice, yet health professions students have limited opportunities to lead imaging-based research. Furthermore, traditional anatomy education rarely exploits primary imaging data to gain a comprehensive three-dimensional understanding of human structures. To address these challenges, the StudentBody initiative at Oklahoma State University offered students self-scanned MRI data for scholarly activities. StudentBody+ expanded this approach by establishing a community-based imaging repository, facilitating broader research engagement.
Methods: StudentBody enabled students to undertake MRI scans of themselves for research and educational model creation. Scanning capacity and financial constraints led to development of StudentBody+, enabling students to access the deidentified, donated medical imaging scans. Research is student-led, with faculty mentorship, guiding IRB protocol development, imaging processing, and data analysis. Privacy and security measures included pseudonymization of scans and restricted access protocols.
Results: The initiatives initially supported three student-led imaging projects. Students applied novel imaging techniques and processing pipelines. Early outcomes include multiple conference presentations and 3D-printed anatomical models for teaching dissemination. Imaging analysis tutorials and remote-access tools enhanced student autonomy. Preliminary findings suggest improved anatomical comprehension, increased research engagement, and higher research output.
Conclusions: StudentBody empowers students in health professions to investigate questions they conceive using their own MRI scans. StudentBody+ markedly expands opportunities for student research by forming a repository of donated imaging datasets. These approaches foster opportunities and a culture of independent inquiry in medical education, bridging the gap between classroom learning and biomedical research.
Acknowledgements: Dr. Alexander Claxton, OSU COM CT Imaging Lab
Introduction
Anatomy-based research and education have the potential to intersect powerfully through advancements in medical imaging. Medical education is undergoing a significant transformation, shifting from traditional, passive learning methods to more experiential and competency-based models. Anatomy education, a fundamental component of medical training, has traditionally relied on cadaver dissections and textbook-based learning. While dissection especially provides primary insights into human structure, these approaches are often limited in scope, accessibility, and real-world applicability. In particular, students frequently struggle with translating two-dimensional textbook images or cadaveric dissections into a comprehensive three-dimensional understanding of anatomical structures. Further into their programs, students interested in anatomy-focused fields such as OMM, orthopedics, rheumatology, surgery, and radiology have scant opportunities for self-directed primary research during their rotations. Some residencies require the completion of research clerkships. Integrating medical imaging, such as magnetic resonance imaging (MRI) and computed tomography (CT), presents an opportunity to bridge this gap by offering dynamic, real-time anatomical visualization. However, financial and logistical barriers often restrict student access to imaging resources, limiting their ability to engage in self-directed anatomical research.
At Oklahoma State University we launched the StudentBody initiative in 2022, providing students with IRB-approved access to self-scanned MRI data for independent research and educational projects to address these challenges. The pilot phase demonstrated the potential of self-directed imaging research, but scan-time and financial constraints highlighted scalability limitations. As a result, we introduced StudentBody+ in 2025, which vastly augments self-scanning with a community-based imaging repository, in which students gain access to de-identified medical scans donated by volunteers. This new model significantly expands research opportunities by removing the need for in-person imaging while maintaining data security and privacy through rigorous de-identification protocols.
StudentBody enables students to conceive, conduct, and create research and educational resources based on direct MRI scans of themselves. By providing cost-free access to an expanding imaging database, StudentBody+ democratizes medical imaging research and fosters an active learning environment where students can engage in real-world anatomical investigations.
The primary objective of StudentBody+ is to facilitate independent student-led research and educational projects by providing unrestricted access to existing medical imaging data. Secondary objectives include evaluating the impact of accessible medical imaging on student engagement, anatomical learning outcomes, and research productivity. Two key hypotheses guide this evaluation: (1) participants will report improved understanding of anatomy, function, and clinical correlations compared to their previous experience with traditional learning methods, and (2) the implementation of StudentBody+ will increase scholarly output, including student-authored publications, conference presentations, and the development of educational tools such as 3D anatomical models. Our increased sample size from StudentBody+ will allow us to test our hypothesis for statistical significance with survey methods in the future. Here, we report our initial results, which at this stage anecdotally inform our guiding long-term hypotheses and raise the promise of quantitative study design for future testing.
This paper outlines the design and implementation of the StudentBody and StudentBody+ programs, evaluates their early outcomes, and discusses their potential to propel anatomy education and research engagement in medical training.
Methods
StudentBody (2022–Present): The initial phase recruited students for two MRI scanning sessions per year with three initial participants, and two since. Each student, sometimes with research partners, developed their own research or educational project. After formulation, students created Institutional Review Board applications for their research. Through the IRB application, evaluation, and approval, students learned the other side of the research process which will inform their future participation in clinical studies as physicians. Once IRB protocols are complete and approved, the students undergo MRI acquisition at the OSU Biomedical Imaging Center, at the Hardesty Center for Clinical Research and Neuroscience. Subjects and partnering students processed the images series at (1) the OSU COM CT Imaging Lab (OSU Tulsa), and (2) both remotely via Zoom and in person on computers at OSU COM Cherokee Nation. Mentors guided students to appropriate software packages based on their project goals. Then students followed internally created tutorials for software packages available in lab (Horos, Avizo, SlicerMorph) while giving access to real-time instructor feedback to maximize student and instructor productivity. After the initial software learning phase, each project becomes entirely student-led with lab staff available for support. Students quickly become autonomous with their image processing pipelines.
StudentBody+ (2025–Present): To overcome financial limitations and scanning constraints, StudentBody+ allows OSU students, staff, and volunteers from the larger community, to donate their existing medical imaging scans to a secured repository. Health professions students can use these deidentified scans for independent research projects.
Participant Recruitment and Data Collection
Through email, flyers, and class announcements, individuals are notified about the program and HIPAA regulation 45 CFR 164.524 [Access of individuals to protected health information].1 This statute protects an individual’s right to receive a copy of their medical records, including medical imaging. Once participants collect their existing medical scan (most frequently as a CD), they then drop it off at a secured location at either OSU Center for Health Sciences (Tulsa) or OSU COM Cherokee Nation (Tahlequah). After signing a consent form and sharing optional demographic information via a survey, their role in the repository is complete. At any point, participants can remove their medical imaging data from the repository by contacting the organizers.
Student Access and Research Project Development
A database of shared scans is maintained, and access is only given to the heads of StudentBody+. At no point will health professions students have unfettered access to this secured repository of scans. Students at OSU can conceptualize a project and reference a deidentified spreadsheet of available scans to assess the feasibility of their ideas. Students have open access to the scan regions and types available for their research (i.e. left shoulder MRI or right knee CT).
After developing a plan and presenting it to the StudentBody+ coordinators, the student will be given access to only the necessary deidentified scans for their project, pending approval by the principal investigator. Project proposals are evaluated based on feasibility, engagement level, and alignment with program objectives. The goal is to approve as many projects as possible to maximize participation.
Data Security and Privacy Measures
Each scan is deidentified through pseudonymization. All identifying information is removed and a randomly selected 6-digit numeral is attached to the scan. DICOM library (Dicomworks), a free DICOM de-identification tool has been tested and demonstrated 100% accuracy with default settings, is used to complete this process.2,3 The master key associating codes with identifying information is only available to the head of OSU COM CT Imaging Lab and the coordinators of StudentBody+. It is stored behind two secured doors in OSU-Tulsa Anatomy and Cell Biology offices.
Participants can share demographic information (age and sex) with health professions students. If available, this demographic information will only be shared with students whose research requires this data, and are chosen to receive access to that particular scan for their project.
Results
StudentBody Outcomes
Quantitative Findings:
Three students generated MRI scans. MRI scan regions included the head and brain, neck, hand and wrist, and lower limb. Three students generated a poster project at OSU Research Days 2024.4 One student generated a 3D virtual and printed model of their visual system, and another student generated a musculoskeletal model of their lower limb. Students presented at both OSU Research Days and Anatomy Connected 2024.4,5 Five health professions students participated in the analysis of this imaging data, and five students have been recruited into their research projects based on presentations of the program.
Standardized Software Training Materials:
We have generated comprehensive software tutorials for Horos (Horos Project, Geneva, Switzerland), Avizo (Thermo Fisher Scientific, version 2020), and SlicerMorph.6 Our lab has also written guides for students to remote access the lab computers to promote open accessibility and how to complete an IRB protocol. Students always have the option of discussing steps with an instructor. However, by first working through the lab materials, instructors can mentor more students and students are able to further develop their problem-solving skills.
StudentBody Case Studies:
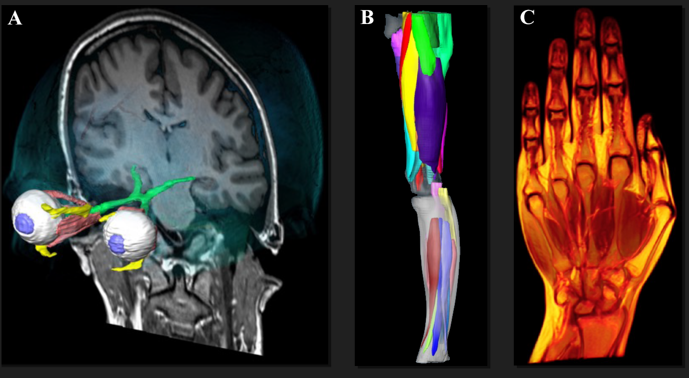
Figure 1: Case study results from StudentBody. (A) Segmented visual system including extra-ocular muscles from Avizo. (B) Posterior-medial view of segmented right lower limb muscles from MRI in Avizo. (C) Coronal slice through the palmar view of wrist MRI in Horos.
1. Brain and 3D Visual System Model: An anatomically accurate 3D model of the visual system was created from a head MRI (Fig. 1A). The resultant 3D print is used in OSU’s Nervous System course to both enhance learning for enrolled students by enabling tactile investigation of this delicate system, and demonstrate the potential of student-led anatomical research in medical education. The subject granted their permission to use their brain MRI in the Nervous Systems labs. Students reported enjoyment at being quizzed on structures rendered in 3D cutaway videos (Horos), of hundreds of orthogonal sections.
2. Musculoskeletal Model of the Lower Limb: A student doctor fulfilled their research rotation by developing a novel segmentation technique that enables non-contrast muscle identification from MRI (Fig. 1B). Their lower limb model has catalyzed further research into subject-specific muscle forces and bone response in female athletes. Further research involving application the of these forces through finite element (stress and strain) analysis with measurement-modified bone, joint forces, and attachment constraints is underway.
3. Carpal Joint Spacing Study in Autoimmune Disorders: A team of student doctors investigated differences in carpal joint spacing in individuals with childhood-onset autoimmune diseases versus healthy controls (Fig. 1C). Further control and affected students are joining this project to increase the sample size for statistical robustness and carry the project long past its origin. Early data was presented at the annual OSU Research Week.4
StudentBody+ Outcomes
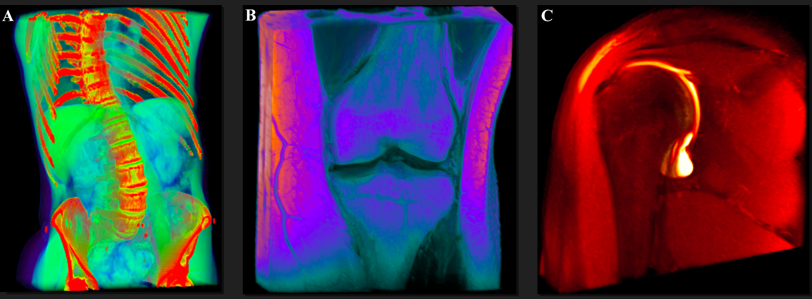
Figure 2:Horos renders from StudentBody+. (A) Rendering of a torso contrast CT scan from patient with scoliosis, anterior view. (B) Anterior coronal section view of a left knee MRI. (C) Coronal section of a right shoulder MRI.
Preliminary Engagement:
Within one week of completing the receiving infrastructure and with no widespread announcements, the repository officially obtained five scans. Scans include two torso contrast CT scans (Fig. 2A), thorax MRI, knee MRI (Fig. 2B), and shoulder MRI (Fig. 2C).
Infrastructure:
The project has obtained open-ended (not time restricted) IRB approval under protocol number 2024146, developed secured data storage, and a donation and de-identification process, as detailed in the Methods. We also created a workflow for non-isometric scans common in medical imaging. Traditionally, medically necessitated MRI involves 2D scans acquired in multiple planes. In these scans, only one orthogonal plane is in high resolution, creating difficulties for researchers attempting 3D reconstructions. Our lab has developed a methodology predicated on the SMORE algorithm to overcome this limitation.7 The algorithm uses machine learning from the high-resolution MRI slices to enhance the clarity of the lower-resolution, out-of-plane MRI images derived from the high-resolution field of view (in prep).
Discussion
The StudentBody and StudentBody+ initiatives align with experiential learning theory by transforming students from passive learners into active knowledge creators.7 Traditional anatomy education often relies on memorization and static images, which do not adequately prepare students for the complex three-dimensional spatial reasoning required in medical practice. These projects continue to assess the likelihood that students will develop a deeper and more applied understanding of human anatomy by directly engaging with medical imaging data and learning to manipulate and analyze it. We anticipate that this model will bridge gaps between theoretical knowledge and practical application, fostering research-driven mindsets among health professions students. Furthermore, StudentBody+ supports competency-based medical education by allowing students to set their learning objectives, engage in self-directed research, and produce meaningful educational outputs such as 3D anatomical models and biomechanical analyses.10 This experiential approach enhances critical thinking and problem-solving, better equipping students for clinical careers and clinical research participation as physicians.10
A primary goal of these projects is to increase student engagement in self-directed research. Early outcomes from the StudentBody pilot phase support this expectation, as seen in engagement in research clerkships, the number of student-led projects, the range of research topics pursued, and the level of independence students demonstrated in executing their studies. StudentBody+, which expands data access through a repository of donated medical imaging scans, is expected to further enhance participation by removing the logistical and financial constraints of acquiring new imaging data. By allowing more students to engage in imaging-based research without the need for in-person scanning, StudentBody+ fosters a more inclusive and scalable research ecosystem. Tracking the number of students proposing and completing research projects and analyzing participation trends over time, will further access the validity of this hypothesis.
The first hypothesis—that participants using StudentBody+ will report an improved understanding of anatomical structures compared to their peers—is grounded in the unique educational benefits of hands-on imaging research. StudentBody has anecdotally demonstrated how active engagement with imaging data improves anatomical comprehension. The creation of 3D models, such as the visual system reconstruction and musculoskeletal segmentation, highlights how students can develop a more sophisticated understanding of spatial relationships and anatomical variations beyond what textbooks and cadaveric dissections offer. Future studies will aim to quantitatively measure this impact by comparing performance metrics, such as anatomy course GPAs, structured student surveys, and evaluations of spatial reasoning skills, between students who participate in StudentBody+ and those who do not.
The second hypothesis—that implementing StudentBody+ will increase scholarly output, including publications, conference presentations, and the development of educational tools—is reflected in early successes, but for research output has yet to be tested against baselines of individual and collective student research productivity at OSU. Already, StudentBody participants have presented research at OSU Research Days and Anatomy Connected 2024.4,5 Their 3D anatomical models have been incorporated into coursework to aid in student learning. StudentBody+, with its larger repository of imaging data, will further drive research productivity by providing a richer dataset for inquiry. Tracking of research outcomes—including peer-reviewed publications, conference abstracts, and student-developed educational materials—will be a key metric in testing this hypothesis.
Compared to external medical imaging repositories, StudentBody+ offers distinct advantages. Many curated databases, such as those managed by large institutions, require expensive subscriptions or limit access to select researchers.11 StudentBody+ democratizes access by providing OSU students with cost-free, institutionally supported imaging data, allowing a broader range of students to pursue research. However, challenges remain. Reliance on voluntary donations means scan availability is variable, leading to potential gaps in demographic representation and pathology diversity. These limitations could introduce biases in research findings, making careful dataset expansion and rigorous project selection essential for maintaining the program’s robustness.
Additionally, technical and ethical challenges must be addressed to ensure the long-term success of StudentBody+. Variability in scan parameters—from differences in imaging protocols across healthcare providers—poses difficulties in standardizing data for research. The program is implementing reconstruction methodologies, such as non-isometric scan enhancements, to improve image uniformity and enhance the reliability of anatomical models thus mitigating the issues with data standardization. Ethical concerns also play a crucial role. While current pseudonymization protocols effectively remove all identifiable data, ongoing evaluation is necessary to ensure compliance with evolving privacy regulations.
The scalability of StudentBody+ remains a key focus. The program has the potential to expand beyond health professions students by fostering interdisciplinary collaborations with fields such as engineering, biomedical sciences, and data analytics. These partnerships could enhance imaging analysis capabilities, leading to innovative applications in biomechanics, prosthetic development, and disease modeling. Institutional support and external funding will be crucial for sustaining and growing the initiative. Conference presentations are showcasing the program’s impact and attracting interest from institutions seeking to adopt similar models.5
A crucial component of future development involves longitudinal tracking of StudentBody+ participants. Proposed metrics include:
● Comparing anatomy course GPAs between StudentBody+ participants and non-participants,
● Assessing residency match rates for students who engaged in imaging research,
● Monitoring ongoing research engagement among program alumni.
By establishing these tracking mechanisms, StudentBody+ can generate empirical evidence of its educational impact, further supporting its case for broader institutional adoption.
Conclusion
StudentBody+ represents a novel and scalable approach to integrating medical imaging research into anatomy education. The initiative addresses critical gaps in traditional learning methods by providing cost-free access to imaging data and fostering student-driven research. While early outcomes demonstrate feasibility and significant educational benefits, ongoing refinement, ethical considerations, and strategic expansion will be essential for maximizing its long-term impact. As the program evolves, it serves as a model for competency-based medical education, encouraging other institutions to adopt similar approaches to enhance research engagement and clinical preparedness among health professions students.
References
1. Health Insurance Portability and Accountability Act (HIPAA), Access of individuals to protected health information. 45 CFR §164.524 (2003). Published 2003.
2. Dicomworks Project. DicomWorks - Free DICOM software. Accessed February 26, 2025. Available at: http://www.dicomworks.com
3. Aryanto KY, Oudkerk M, van Ooijen PM. Free DICOM de-identification tools in clinical research: functioning and safety of patient privacy. Eur Radiol. 2015;25(12):3685-3695. doi:10.1007/s00330-015-3794-0
4. Nees K, McKenzie T, Hartsell L, Simmons K, Snively E. 2024. MRI-based morphometrics of hand+wrist joint spacing in a patient with Juvenile Idiopathic Arthritis. Poster presented at: OSU-CHS Research Week; February 2024; Tulsa, OK.
5. Pennings AN, Snively E, Emmert R, McKenzie T, Nees K, Ray K, LeFleur F, Simmons WK. “StudentBody:” translational learning and research for the student body through medical imaging [abstract]. Anat Sci Educ. 2024;17(S1):145-146.
6. Rolfe S, Pieper S, Porto A, Diamond K, Winchester J, Shan S, Kirveslahti H, Boyer D, Summers A, Maga A. SlicerMorph: An open and extensible platform to retrieve, visualize and analyse 3D morphology. Methods in Ecol Evol. 2021;12(10):1816-1825. doi:10.1111/2041-210X.13669
7. Zhao C, Dewey BE, Pham DL, Calabresi PA, Reich DS, Prince JL. SMORE: A Self-Supervised Anti-Aliasing and Super-Resolution Algorithm for MRI Using Deep Learning. IEEE Trans Med Imaging. 2021;40(3):805-817. doi:10.1109/TMI.2020.3037187
8. Kong Y. The Role of Experiential Learning on Students' Motivation and Classroom Engagement. Front Psychol. 2021;12:771272. Published 2021 Oct 22. doi:10.3389/fpsyg.2021.771272
9. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. doi:10.3109/0142159X.2010.501190
10. Jacob SA, Power A, Portlock J, Jebara T, Cunningham S, Boyter AC. Competency-Based Assessment in Experiential Learning in Undergraduate Pharmacy Programmes: Qualitative Exploration of Facilitators' Views and Needs (ACTp Study). Pharmacy (Basel). 2022;10(4):90. Published 2022 Jul 26. doi:10.3390/pharmacy10040090
11. Edgar HJH, Daneshvari Berry S, Moes E, et al. New Mexico Decedent Image Database. Office of the Medical Investigator, University of New Mexico; 2020. doi:10.25827/5s8c-n515