QUALITY IMPROVEMENT IN COLONOSCOPY AND LOW VOLUME ENDOSCOPISTS: A SINGLE CENTER EXPERIENCE
William G. Simpson, M.D, Department of Rural Health - Gastroenterology, Oklahoma State University College of Osteopathic Medicine
Abstract
Colonoscopy is accepted as a means to screen patients for colon cancer and adenomatous colon polyps. To make recommendations to patients and primary care providers with clinical confidence performed colonoscopy should be performed at a high quality level. We report the impact of implementation of an ongoing colonoscopy quality improvement initiative at a single institution on the performance of low volume endoscopists. The program, based on recognized national standards, yielded marked improvement in the performance of these providers. Adenoma detection rate actually improved in both the high volume and low volume endoscopists. Procedure volume is a poor predictor of competence in endoscopy, but education and monitoring of quality metrics helped low volume endoscopists meet performance standards.
Introduction
Colorectal cancer results in nine percent of the cancer deaths reported in the United States annually, and roughly one third of patients diagnosed with colorectal cancer die of the disease 1. Screening efforts focus on the early detection of treatable and curable cancers and on the identification and removal of adenomatous colon polyps. Interruption of the adenoma-carcinoma sequence of development of colorectal malignancy is possible if adenomatous polyps are removed while still benign. The National Polyp Study prospectively followed a large population of patients referred for colonoscopy where polyps were removed, and demonstrated a 53% reduction in mortality from colorectal cancer 2. Nishihara et al. 3 reviewed data from the Nurses' Health Study and the Health Professionals Follow-up Study and demonstrated a reduction in the incidence of colorectal cancer of 53% after colonoscopy with polypectomy and 56% in the ten years after a negative screening colonoscopy. There was a 68% reduction in death from the disease after a screening colonoscopy. Among individuals of average risk of the development of colorectal cancer, screening colonoscopy identifies large adenomatous polyps and cancer with high sensitivity (85-95%) and resulted in the prevention of 22-24 deaths from the disease per 1000 forty year old patients 4. Colonoscopy is recognized by the US Preventive Services Task Force as an acceptable means of screening for colon polyps and cancers 5. Because it is sensitive, and offers the benefits of both polyp identification and polypectomy at the same time, colonoscopy is recommended as the screening test of choice by US Multi-Society Task Force of Colorectal Cancer 6.
As is apparent from the discussion above, the primary goal of colorectal cancer screening is the identification and removal of benign adenomatous polyps. The appropriate utilization of screening colonoscopy has become a point of emphasis among both primary care providers and specialists, notably gastroenterologists and surgeons (general and colorectal). Although there are differing opinions between these groups as to the requirements for adequate training to perform endoscopy, it is clear that competency in colonoscopy is not solely determined by volume of procedures performed 7,8,9,10. If colonoscopy is performed properly and polyps are removed both patients and primary care providers can have confidence that every reasonable effort has been made to prevent this malignancy. Quality indicators for colonoscopy have been established to allow assessment of the performance characteristics of providers 11,12. While such quality indicators are used in ongoing credentialing and allow one to compare providers using defined metrics, they may well also serve to stimulate performance improvement by individual endoscopists. We report the impact of implementation of a quality improvement program on the performance of endoscopists at a single center.
Methods
During 2017 an endoscopy quality improvement program was initiated at Northeastern Health System (Tahlequah, Oklahoma). Based on metrics reviewed and proposed by the American Society for Gastrointestinal Endoscopy and the American College of Gastroenterology 11,12 a panel of quality indicators was developed and agreed to by all providers of endoscopy at the institution (Table 1).
TABLE 1
Colonoscopy Quality Parameters
| Parameter |
Standard Threshold |
| Frequency with which bowel preparation is good or excellent (bowel prep) |
> 85% |
| Frequency of photodocumentation of cecal landmarks (cecal intubation) |
> 95% |
| Frequency with which withdrawal time is > 6 minutes (withdrawl time) |
≥ 98% |
| Frequency of adenomatous polyp detection in screening patients (adenoma detection rate or ADR) |
> 25% |
This process involved education of each provider involved as to the rationale underlying the program as well as the definition of each parameter to be studied. Endoscopists were provided copies of the standards published by professional societies and, after discussion the definition of quality indicators were agreed upon. While data was collected on all endoscopic procedures (esophagogastroduodenoscopy, colonoscopy and endoscopic retrograde cholangiopancreatography) only the data for colonoscopy is reported here. The outcome of each parameter was collected for every colonoscopy performed and was summarized monthly. Each endoscopist received reports of their individual performance broken down by quarter including reinforcement of the agreed to threshold standards of performance. These quarterly reports served to provide periodic education as well as incentive to satisfy performance standards to the involved physicians. For the purpose of this study providers were separated into low volume and high volume groups based simply on the number of colonoscopies performed, and data was extracted for the 18 months following initiation of the program. While quarterly data was reviewed, pooled data from the providers in both volume groupings are reported from the initial collection quarter and the final collection quarter. Three parameter thresholds were universally achieved by all providers across the time period studied and are not reported further: failure to perform a "time out" (standard < 2%), presence of an updated history and physical before starting the procedure (standard > 98%) and preoperative marking of the surgical site (standard 100%).
RESULTS
Over the 18 month study period a total of 1,589 colonoscopies were performed. The providers involved were classified as high volume (one provider) or low volume (two providers) based on the number of colonoscopies performed. The high volume provider performed 1,418 (89.2%) studies (78.8 per month) while the low volume providers performed 171 (10.8%) studies (average 4.75 per month per provider). No perforations occurred during the study period. Initially the low volume providers fell below the performance standard and were well below the performance of the high volume group for quality of colon preparation (77.4% vs. 98.6%), rate of intubation of the cecum (80.9% vs 99.0%), colonoscope withdrawal time (64.3% vs. 99.5%) and adenoma detection rate (15.4% vs. 51.0%)(Table 2).
TABLE 2
Colonoscopy Quality Parameters Reviewed
|
High Volume Provider |
|
Low Volume Providers |
|
Initial |
Current |
|
Initial |
Current |
| Quality of Preparation1 |
98.6 % |
100.0 % |
|
77.4 % |
100.0 % |
| Cecal Intubation2 |
100.0 % |
99.0 % |
|
80.9 % |
96.0 % |
| Withdrawl Time3 |
96.4 % |
99.5 % |
|
64.3 % |
100.0 % |
| Adenoma Detection4 |
51.0 % |
76.5 % |
|
15.4 % |
62.5 % |
LEGEND
Figures reported are percentages of patients studied for: (1) quality of colon preparation either good or excellent (standard 85%), (2) cecal intubation rate (standard >95%), (3) colonoscope withdrawl time of six minutes or more (standard >98%), and (4) adenoma detection rate (standard >25%).
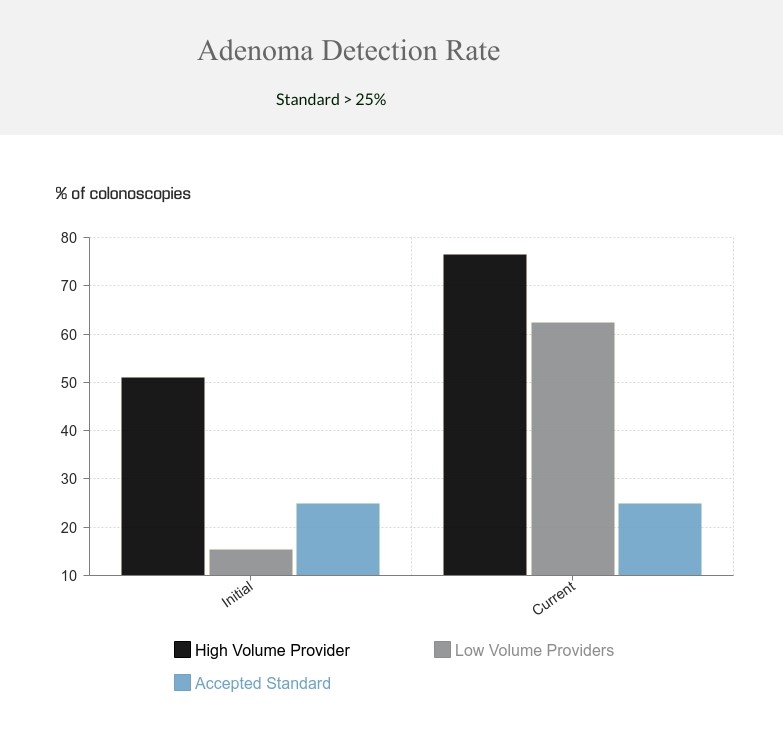
After 18 months of involvement in the quality improvement program the low volume providers demonstrated marked improvement. Performance now exceeded established standards for the quality of preparation, cecal intubation rate and colonoscope withdrawal time (Table 2). Of note, adenoma detection rate improved from 15.4% to 62.5% and now approached that of the high volume endoscopist (Figure).
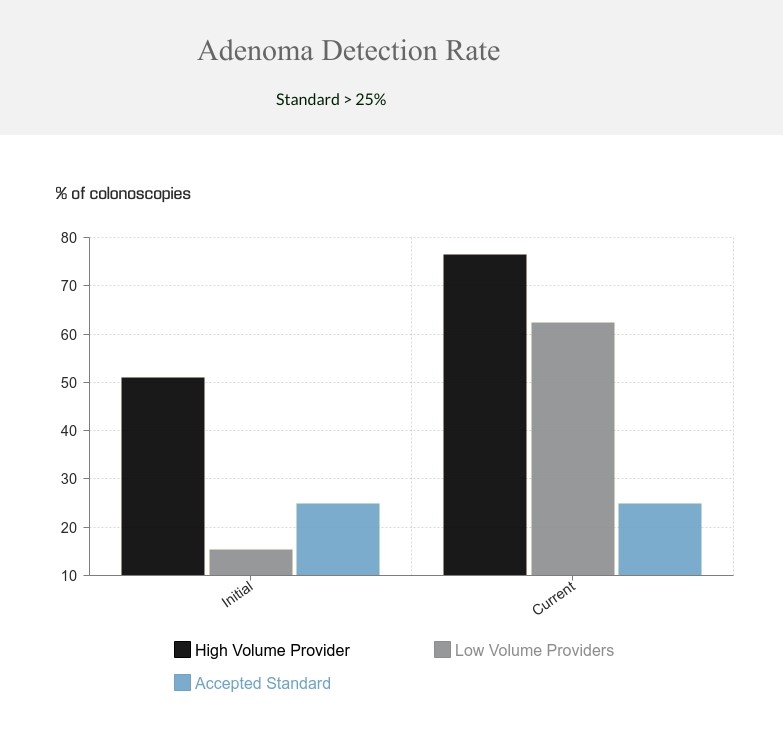
FIGURE
Initial and final adenoma detection rates among high volume and low volume providers involved in a colonoscopy quality improvement program as compared to the performance standard of > 25%.
DISCUSSION
It is clear that the burden of colorectal cancer, currently one on the most common causes of cancer death in Americans 1, can be reduced by appropriate utilization of colonoscopy 2,3. Early detection of colorectal cancers offers opportunity for cure. Greater opportunity lies in the potential to interrupt the development of cancer by endoscopically identifying and removing adenomatous colon polyps thereby truncating the adenoma-carcinoma sequence. This requires not only the timely and appropriate implementation of screening colonoscopy but also performance of a high quality study. A sub-standard screening study in fact exposes patients to an increased risk of developing a disease from which they feel relatively safe.
There remains some element of controversy as to who is best suited to perform screening colonoscopy. Clinical reality is that the volume of patients in need of quality screening necessitates that providers across appropriate specialties be involved. What is clear, however, is that endoscopists must be competent and that competence is not merely dependent upon the volume of colonoscopies performed 13. Providers who are low volume should not be excluded from the endoscopy suite, but should be held to the same quality standards established for all endoscopists. We report the beneficial impact of a quality improvement program in just such regard. Implementation of this a program at our institution was demonstrated to improve the quality of procedures performed by both high and low volume endoscopists. Of greatest significance was the rise in the adenoma detection rate in both high volume (51.0% to 76.5%) and low volume (15.4% to 62.5%) providers. This finding likely reflects the impact of physician education and reinforcement of the need for attention to provision of quality colonoscopy in the screening population. Among the low volume providers an improvement in colon preparation, cecal intubation rate and a more thorough inspection of the colonic mucosa (as inferred by an appropriate withdrawal time) likely all contribute to an improvement in the identification and removal of polyps. An overall improvement in adenoma detection was demonstrated across the study period for all providers suggesting an improved awareness resulting from the program.
We demonstrate that the development and implementation of a quality assurance program in endoscopy improves adenoma detection rate in patients undergoing colorectal cancer screening. The identification and removal of adenomatous colon polyps is key to the process of preventing colorectal cancer. Providers were educated with literature based discussion of the standards employed. Additionally, the concepts were reinforced daily as procedures were done and periodically as results were reviewed with each provider. This education and insight appears to result in performance improvement not only in endoscopists who were not previously meeting standards but also in higher volume providers who were.
These results are limited by the fact that only a single center was involved and the fact that the number of providers of endoscopy were small. The change demonstrated at a single rural center is encouraging. Assessment of the performance of a quality improvement program at a larger urban center would be of value.
An ongoing process of performance review and improvement such a program is a vital component of the maintenance of quality as well as one component of the ongoing assessment of provider competence 14. Ultimately it is the patient who benefits from improvement in the quality of colonoscopy delivered and the resultant reduction in risk of development of colorectal cancer.
Key words: colonoscopy, quality improvement, adenoma detection rate, colon cancer screening
Acknowledgements: The author wishes to acknowledge the assistance of Hollie Carroll, R.N., CGRN, Endoscopy Clinical Coordinator, Northeastern Health System.
REFERENCES
1. Siegel R, Miller K, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69(1):7-34.
2. Zauber A, Winawer S, O'Brien M, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366(8):687-696.
3. Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 2013;369(12):1095-1105.
4. Knudsen A, Zauber A, Rutter C, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016;315(23):2595-2609.
5. Lin J, Piper M, Rutter C, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016;315(23):2576-2594.
6. Rex D, Boland C, Dominitz J, et al. Colorectal cancer screening: recommendations for physicians and patients from the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2017;153(1):307-323.
7. Wexner S, Litwin D, Cohen J, et al. Principles of privileging and credentialing for endoscopy and colonoscopy. Gastrointest Endosc 2002;55(2):145-148.
8. Wexner S, Eisen G, Simmang C, et al. Principles of privileging and credentialing for endoscopy and colonoscopy. Dis Colon Rectum 2002;45(2):161-164.
9. American Society for Gastrointestinal Endoscopy Standards of Practice Committee. Methods of granting hospital privileges to perform gastrointestinal endoscopy. Gastrointest Endosc 2002;55(7):780-783.
10. Joint Statement by the American Society for Gastrointestinal Endoscopy, the Society of American Gastrointestinal Endoscopic Surgeons, and the American Society of Colorectal Surgeons. Principles of privileging and credentialing for endoscopy and colonoscopy. Gastrointest Endosc 2002;55(2):145-148.
11. Rizk M, Sawhney M, Cohen J, et al. Quality indicators common to all GI endoscopic procedures. Gastroinest Endosc 2015;81(1):3-16.
12. Rex D, Schoenfeld P, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015:81(1):31-53.
13. Wexner S, Garbus J, Singh J, et al. A prospective analysis of 13,580 colonoscopies: reevaluation of credentialing guidelines. Surg Endsoc 2001;15(3):251-261.
14. American Society for Gastrointestinal Endoscopy Standards of Practice Committee. Renewal of and proctoring for endoscopic privileges. Gastrointest Endosc 2008;67(1):10-16.